A Breakdown on Migraines

Key Takeaways
Do you ever get a throbbing or pulsing sensation on one side of your head? Is it often accompanied by feelings of nausea, dizziness, or vision disturbances like seeing flashing lights that aren't there? If so, you may be experiencing a migraine headache.
There are several types of headaches: cluster headaches, tension headaches sinus headaches, hormone headaches, caffeine headaches... the list is extensive. And migraine headaches may be one of the most painful ones on the list. This type of headache is more than your average headache, and a lot more difficult to deal with if you have chronic migraines. While you've likely said, "I have a migraine" at some point in your life, do you know what it is, how to recognize it, and what you can do to ease the ache?
What are Migraines?

The first thing to note is that migraines are a more common type of headache and more prevalent than you'd imagine. According to the American Migraine Foundation, more than 36 million people in the United States suffer from migraine headaches.
But, what are they? Migraines are a neurological condition that causes severe headaches. Unlike other primary headache pain, migraines cannot always be cured by over-the-counter medication and sometimes require diagnosis by a healthcare professional. However, a review found that some medications like ibuprofen may help relieve head pain associated with headache disorders like migraines. Certain acetaminophen and triptans may also help some people.
All migraine headaches aren’t the same either, there are many different types of migraines that appear in different people and may occur at different stages of their lives. There are silent migraines, a type of migraine that occurs without any head pain. They're typically present among those who get migraine auras (more on that below!) and go hand-in-hand with aura symptoms including nausea and dizziness. There are also chronic migraines, menstrual migraines, ocular migraines, retinal migraines, and abdominal migraines. There's also a rare disorder called hemiplegic migraine, in which you also experience weakness on one side of the body.
The Warning Signs

Migraine attacks can sometimes come up quite suddenly and without warning, but there are sometimes triggers you can learn to be wary of. Some people experience warning signs before they experience a migraine. Migraines often have neurological symptoms, like visual disturbances, vertigo, blind spots, dizziness, and nausea—often similar to symptoms of a stroke.
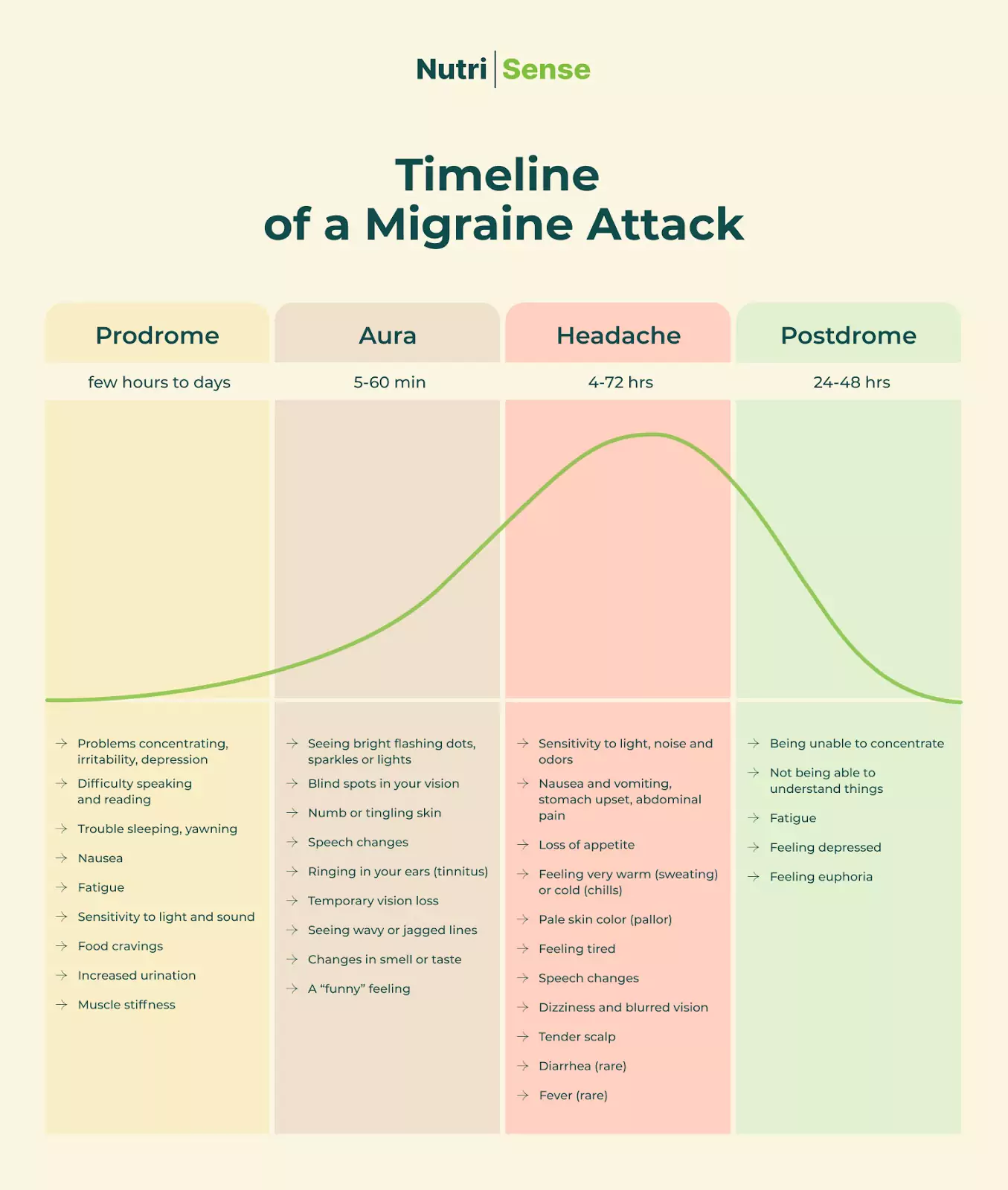
Some people may experience what is known as a migraine aura in lieu of, or before the migraine pain. Migraines progress through four stages in some patients. These are prodrome, aura, attack, and postdrome. As research has found, the timeline of a migraine attack usually looks something like this:
Prodrome
The prodrome stage begins one to two days before the migraine begins. People who experience this stage of their migraine headaches may experience the following symptoms and warning signs before the migraine pain sets in:
- Neck and back stiffness
- Changes in mood
- Constipation
- Fluid retention
- Yawning
- Frequent urination
- Food cravings or loss of appetite
- Bloating
- Sensitivity to light, sound, or smells
- Increased thirst
Aura

Auras are symptoms of your nervous system that occur before a migraine, and sometimes during one. Usually, auras are visual and last anywhere from a few minutes to an hour. They can affect speech, smell, taste, or touch. Some people experience more frequent migraine auras than others. Headaches that are specifically migraines with brainstem auras start on one side of the head, in the lower part of the brain or the brainstem. Approximately 15 to 20 percent of people with migraines experience aura symptoms that may include:
- Visual disturbances like seeing “stars”
- Blind spots
- Muscle weakness
- Loss of vision
- Trouble speaking
- Face or body numbness
- Pins and needles
- Ringing in the ears
Attack (Headache)
The attack is the migraine itself. Migraine attacks last from a few hours to three days, but the entire experience may last much longer and is often quite challenging to deal with. Every case is different and the frequency with which migraines occur varies on a case-by-case basis. Some people experience migraines very rarely, while some suffer from them multiple times a month. Those suffering from a migraine may experience:
- Pain on one or both sides of the body or sides of the head
- Throbbing pain in the temples
- Light, touch, smell, and sound sensitivity
- Nausea
- Vomiting
- Clammy skin
- Pain in the front of the head
Postdrome

Postdrome is the period of time that a person that has suffered a migraine recuperates. The postdrome stage usually lasts for about a day after the attack. The postdrome stage is sometimes called a 'migraine hangover,' and the symptoms include:
- Fatigue
- Crankiness and mood swings
- Intense food cravings
- Loss of appetite
- Muscle weakness and joint pain
- Feelings of happiness
What Causes Migraines?

Research on what causes migraines is still ongoing, but so far, environmental factors, imbalances in brain chemicals, changes in the brainstem’s interactions with the trigeminal nerve, serotonin, and genetics seem to factor into the equation.
Approximately 80 percent of people who suffer from migraines have a relative who does as well, which means family history and genes are important factors. The hormonal shifts that are linked to migraines are also why women are two to three times more likely to suffer from migraines than men.
While there is no known cause to pinpoint for this type of headache, there are certain triggers that you can use to see whether you suffer from them. Known migraine triggers include:
Certain Foods: Eating certain foods may trigger migraines in some people. Several foods may trigger a migraine attack, and it often depends on your body. Some of the most common migraine-triggering foods include chocolate, cheese and other dairy products, artificial sweeteners like aspartame, caffeine, and cured meats.
Some Food Additives: Food additives like nitrates, histamine, and monosodium glutamate are triggers for some people.
Certain Drugs: While over-the-counter medication can be helpful for easing the pain from migraine attacks, some people may experience rebound headaches or medication overuse headaches from certain drugs. Some of these include aspirin, nitrates, triptans, acetaminophen, ibuprofen, naproxen, and codeine.
Stress: People suffering from prolonged stress are more prone to migraine attacks. Stress releases chemicals in your brain that cause changes in your blood vessels, which may result in a migraine.
Hormonal Changes: Women who suffer from migraines may notice that their headaches happen during their period, during ovulation, during pregnancy, or during menopause due to the hormonal shifts in their bodies.
Sleep Changes: Changes in sleeping patterns may cause migraines to occur. Getting too little or too much sleep can also determine how frequently you get migraine attacks if you have chronic migraine issues.
Physical Activity: Strenuous physical activity such as intense exercise or sexual activity can trigger a migraine.
Sensory Stimuli: Bright or flashing lights, loud noises, and pungent smells may trigger a migraine. People with migraines tend to avoid environments that may contain sensory overloads, especially if they experience symptoms like visual disturbances.
Alcohol Intake: Drinking alcoholic beverages may trigger some people with migraines.
Caffeine: Drinking too much caffeine, or less caffeine than your body is used to, can trigger migraine attacks or headaches.
Changes in Weather: Changes in barometric pressure or altitude, storm fronts, and winds can all trigger migraines.
Dehydration: Yes, dehydration can trigger migraines just as often as it can trigger other primary headaches.
Smoking: Just like excessive alcohol intake, smoking can also lead to a range of health issues. In fact, smoking tobacco is a common migraine trigger.
Who is Most at Risk of a Migraine?

There is no single cause of migraines and so there are various risk factors to consider. Migraines are genetically linked and so your family history can determine whether you're at risk. If someone in your family suffers from migraines, you will be more likely to develop them.
Women are more likely to get migraines than men due to menstruation and hormonal changes. People who live in high-stress environments or are going through a particularly stressful time in their lives are also more likely to develop migraines.
Doctors diagnose migraines by reviewing medical histories and discussing symptoms of migraines with their patients. They will likely ask you to go into great detail about your headaches, any medical conditions you have or have had, and your family history.
They may also ask you to begin keeping a daily journal of how you feel before, after, and during your migraines to see how long they last and what symptoms they cause. This will help them rule out other conditions and identify possible triggers.
While diagnosing migraines, doctors may run blood tests, MRIs, CT scans, and EEGs to rule out other conditions that might be causing severe headaches.
How Are Migraines Treated?

There is presently no cure, but treating the side effects and symptoms of migraines can help patients manage them. Your doctor may recommend preventive treatments or changes to your diet and lifestyle to help reduce triggers. Working in tandem with a registered dietitian to make lifestyle changes may help prevent migraines from happening as frequently.
Migraine Prevention
Everyone that suffers from migraines has varying triggers and needs, but these are a few preventative tips that may help prevent a migraine or lessen its effects:
- Learn the triggers. Keeping a journal and writing down what was eaten the days before a migraine, what physical activity was done, and even the state of the weather may help prevent future triggers.
- Always stay well hydrated.
- Keep a reliable sleep schedule.
- Identify stress points and manage them with techniques like yoga, meditation, hiking, or breathing exercises.
- Stick to a regular eating schedule and keep note of the foods that were consumed right before a migraine started.
- Medications like blood pressure-lowering medications, botox, anti-seizure medications, and CGRP monoclonal antibodies may be prescribed by doctors to help prevent migraines. Some antidepressants are also an effective preventive measure for migraines in some people.
Some Treatments for Migraines

Migraine treatments may be different for different people. Doctors determine on a case-by-case basis how to help prevent a patient’s migraine and how to treat their symptoms.
- Pain relievers are the most prescribed or recommended treatment for migraines, but often don’t do the trick on their own when fighting migraines. Sumatriptan is one of the more common treatments for cluster headaches as well as migraines.
- Anti-nausea medication may be prescribed by doctors to help fight symptoms.
- Opioid medications are prescribed on a case-by-case basis for those with severe migraine cases.
- Acupuncture may help some people with their migraines. Some doctors may recommend trying acupuncture in tandem with their prescribed treatments.
- Doctors often recommend changes in diet and additions of vitamins and nutrients to their patient’s diets.
- There is some research that suggests magnesium may be a good treatment for migraines. The American Migraine Foundation suggests 400–500 milligrams as a preventive measure.
- Rest in a cool, dark, room. Reducing sensory stimuli may help reduce the pain caused by migraines.
- Applying heat or cold to the back of the neck and temples.
- Some doctors recommend using biofeedback equipment to measure physical tension in the body as a way to prevent stress-related migraines.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Carlee's training at Western Illinois University and an internship at the Memphis VA Hospital lead her to a career in outpatient counseling and bariatric nutrition therapy. In these positions, Carlee realized many of the disease states (upwards of 80%!) her patients experienced were actually preventable. She knew she had to dig deeper into preventative health and has since been passionate about helping people translate this complex glucose data into actionable changes anyone can implement into their everyday lives.


.webp)

