How to Combat Seasonal Depression: 5 Helpful Tips

Key Takeaways
Do you struggle with seasonal depression or the winter blues? This condition, which was first documented by Dr. Norman Rosenthal in the 1980s, is characterized by feelings of depression during the colder and darker months.
While many people may have mood fluctuations at certain times, those who experience seasonal depression may feel significant and persistent dips in mood and mental health. Many factors can contribute to and aggravate seasonal depression.
Fortunately, there are steps you can take to boost your mood and support your well-being during these colder months.
In this article, we share both the factors that affect seasonal depression and five tips that can support your mood.
What is Seasonal Depression?
Seasonal depression takes on a few different names, but it’s most commonly referred to as seasonal affective disorder (or SAD) or the winter blues. SAD is not a diagnostic criterion on its own, but rather it’s a subset of major depressive disorder or MDD that occurs during the winter months.
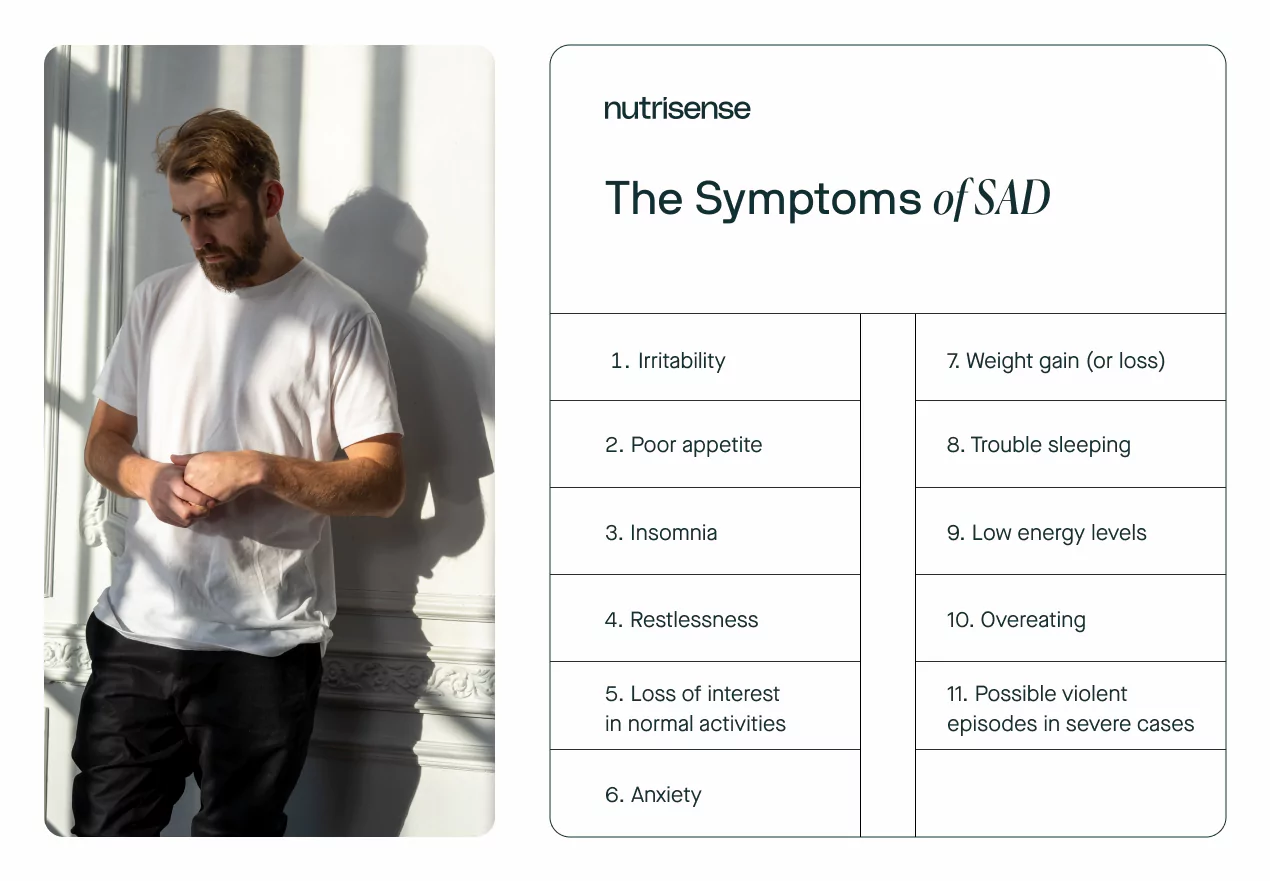
This type of depression most typically occurs during the late fall and winter months. It involves some of the common symptoms of depression, such as significantly low mood, weight gain, low energy levels, over eating, and trouble sleeping.
Additional symptoms of SAD may include:
SAD may occur a bit more often than you’d expect, affecting an estimated six percent of the US population. A milder version of the winter blues may affect up to 14 percent of US individuals.
Interestingly, seasonal depression is shown to affect women as much as four times more than men. Apart from sex, other risk factors can include younger age, living farther away from the equator, and a family history of depression, SAD, or bipolar disorder.
Why Your Mood Feels Low During the Winter Months
So why might your mood drop significantly during the colder months? And why does it seem to affect some people more than others? There are a few factors that may be involved here. Let’s discuss each one of them.
Trouble Regulating Neurotransmitters

Although the activity of neurotransmitters is complex, there are a few that are known to play an important role in the regulation of mood. These include serotonin, norepinephrine, and dopamine. These neurotransmitters are known to be dysregulated in people who have major depressive disorder, and studies indicate that they may also be involved in seasonal depression.
Those who have seasonal depression have trouble regulating serotonin, which is involved in mood regulation. One study found that individuals who experience SAD have five percent higher levels of a protein that helps with serotonin transport.
This protein, called SERT, is involved in transporting serotonin from the area between neurons to inside the neurons. Higher levels of this serotonin transport-related protein can lead to lower serotonin activity, which may, in turn, lead to feelings of depression.
Individuals who do not experience SAD, also called seasonality-resilient individuals, can downregulate their SERT levels during the winter months. As a result, they may be less likely to feel lower moods or feelings of depression.
Lastly, people who experience seasonal depression can also have difficulty with melatonin production and tend to overproduce it. Because melatonin is involved in circadian rhythms, this imbalance can impact people’s circadian rhythms or sleep patterns. The decreased levels of serotonin may aggravate this and further negatively impact the circadian rhythms of people with SAD.
Less Sunlight and Vitamin D Production
During the winter months, you might notice that you stay indoors more often due to harsher temperatures. After all, the idea of spending hours in the biting wind and sub-zero weather isn’t exactly appealing.
The winter months also mean shorter days with less sunlight. These factors may cause people to get significantly less exposure to sunlight on their skin. For people with SAD, this means that their bodies are producing less vitamin D, which may aggravate their symptoms further. In North America, UVB-rich sunlight is naturally scarcer in the winter for many people. This means that vitamin D production is typically already diminished for many who are wintering at certain latitudes.
Tips to Combat Seasonal Depression
Even with all the factors that can aggravate your mood, you can still be proactive in stabilizing your mood and uplifting your spirit! Here are a few tips that can help boost your mood.
1) Try a SAD Light

One of the potential causes of this seasonal form of depression is a lack of natural sunlight during the typical daylight hours. That’s why a common approach to treating seasonal depression involves light therapy.
If you’re not familiar with light therapy, or bright light therapy (BLT), for SAD, it involves using light with certain frequencies to mimic natural light. Research has shown that this can be a promising and effective treatment option for combating seasonal depression.
You can get a light box that emits full spectrum light that’s similar to sunlight composition. People who use this may start by turning it on first thing in the morning to mimic morning sunlight and keep it on their desk at work throughout the day.
Although it is relatively safe, some side effects of light therapy may include:
- Eyestrain
- Increased risk of age-related macular degeneration
- Headaches
- Irritability
- Difficulty sleeping
2) Exercise, Exercise, Exercise!
Exercise can boost your mood by boosting feel-good hormones or endorphins. It can also help modulate the neurotransmitters involved in mood regulation.
Remember how we mentioned that during the winter months, people with SAD have increased levels of SERT? Well, research has shown that exercise can increase levels of serotonin making this an effective way to boost your mood.
Any type of movement can be beneficial to your well-being so you may as well choose one or a few that you like. Try combining a few different ones like walking or dancing throughout the week. You can also pair exercise with some of our other tips on this list, such as using exercise as a way to spend quality time with loved ones.
3) Spend Quality Time with Friends and Family

Even though it can feel like you’re more isolated during the winter months, you’re not. As we’ve already mentioned, SAD is unfortunately quite common so chances are someone you know may experience this too.
Don’t be afraid to reach out to your community or loved ones for additional support during these months. Let them know what’s going on and find ways to spend more quality time with them.
If you don’t relate to those in your immediate surroundings or they find it difficult to understand what you’re going through, you may consider joining a support group that resonates with you.
You can also lean into your therapist, counselor, or healthcare team for support. Simply talking to a licensed professional can help some people feel less burdened and may even point out patterns that may be worsening your mood.
4) Ensure Adequate Vitamin D intake
Vitamin D levels can play a role in low mood, especially during the winter months. Spending time in the sun for a safe length of time is one healthy lifestyle habit that can improve vitamin D levels. However, this may be difficult to do during the winter months.
If you’re not able to get outside as often as you would during the summer, you can increase your vitamin D intake by consuming foods such as:
- Eggs
- Fatty fish such as salmon and sardines
- Organ meat such as liver
- Milk
- Yogurt
Apart from dietary sources, vitamin D supplements may be helpful to increase your levels of this vitamin. However, researchers recommend sourcing the majority of your vitamins and minerals from whole foods when possible. Since moderate chronic intake of vitamin D supplements sufficient to raise serum levels above 50 ng/mL may be linked to increased risk of all-cause mortality, certain cancers, and falls and fractures, it’s important to remember that more isn’t always better. Working with a qualified healthcare professional to guide you in questions of supplementation is crucial.
5) Support Healthy Blood Sugar Levels

Your blood glucose levels may be linked to your mood as well. A study investigating the efficacy of light therapy for mood and insulin resistance in those with type 2 diabetes found a possible link between major depressive disorder, insulin resistance, and blood glucose levels.
Conditions such as insulin resistance can lead to poor glucose response. Insulin signals the body to let glucose into your cells. But if your body isn’t listening to insulin, this can lead to high glucose levels in your blood.
There are many things you can do to support healthier blood sugar levels. For example, eating the right quantity of carbohydrates for your body can prevent higher spikes. Those with SAD often crave carbohydrates during the winter months so finding the right intake can be important.
Getting plenty of exercise, staying hydrated, and taking steps to reduce stress are a few other ways to improve glucose response over time. For more tips that may help stabilize your blood sugar levels, see our article here.
6) Consult a Qualified Mental Health Professional

If these tips have not improved your symptoms over time, you may want to visit a qualified healthcare provider to rule out any other potential health conditions or treatment options.
Only your doctor can prescribe certain treatments such as counseling, cognitive behavioral therapy, or antidepressants. While these options may improve some symptoms for some people, certain medications for treating depression can have other side effects. Newer research has also raised concerns over the efficacy of certain serotonin-regulating medications traditionally thought to treat depression. If you have questions about any of these treatments, consult your medical provider.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Heather is a Registered and Licensed Dietitian Nutritionist (RDN, LDN), subject matter expert, and technical writer, with a master's degree in nutrition science from Bastyr University. She has a specialty in neuroendocrinology and has been working in the field of nutrition—including nutrition research, education, medical writing, and clinical integrative and functional nutrition—for over 15 years.


.webp)

