Stress and Your Period: What's the Connection?

Key Takeaways
Did you know that as many as 35.6 percent of women experience irregular periods? Though there may be many different causes, stress itself plays a big role. Stress can affect your period and overall menstrual cycle and lead to dysmenorrhea or even amenorrhea.
- Amenorrhea: The absence of menstruation, or missed periods
- Dysmenorrhea: Painful menstruation, abnormal bleeding, or PMS symptoms
But how do you know if stress is what’s behind your cycle concerns? What other symptoms can stress cause?
Keep reading to learn how stress impacts your menstrual cycle, where hidden sources of stress might be lurking, and what you can do about it.
Stress and Your Menstrual Cycle

When your body is under higher amounts of chronic stress, your period isn’t the only part of your menstrual cycle likely to be affected. High stress levels may lead to ovulatory dysfunction and changes in both your follicular and luteal phases of your cycle. How does stress do this exactly?
Stress can impact women’s health through the hypothalamic-pituitary-gonadal (HPG) axis. This axis regulates a great deal about hormone balance throughout the entire menstrual cycle. HPG axis dysfunction may cause menstrual irregularities and even infertility in some cases.
How Too Much Stress Damages Women's Health
According to the American Psychological Association (APA), women are around 30% more likely than men to experience the symptoms of chronic stress. Women’s bodies may have some unique responses to stress.
As you may already know, high stress levels may raise cortisol. Cortisol, your primary stress hormone, influences estrogen, progesterone, and even thyroid hormone. Stress also interacts with something called kisspeptin, which is a peptide that regulates reproductive function.
Kisspeptin is a critical regulator of the HPG axis by stimulating hypothalamic gonadotrophin releasing hormone (GnRH). During chronic stress, changes in kisspetin signaling can negatively impact ovulation.
Are you Experiencing High Stress Levels?

Stress is any type of pressure applied to your body and it’s not always bad. What your body does to adapt to the stress is called a stress response. But how much stress is too much? And what counts as stress?
Acute stress is short-term stress that goes away quickly, and is related to your fight-or-flight response. This stress can occur as you slam on the brakes in your car, have to meet a deadline, or have a fight with your friend. Excitement and anticipation may also cause acute stress reactions in your body.
On the other hand, chronic stress can go on for weeks, months, or longer. Chronic stress can lead to more serious health problems.
Here are some potential sources of stress that can affect your health and well-being:
- Emotional, social, or psychosocial stressors
- Nutritional imbalances, including glucose imbalances
- Under-exercise or over-exercise
- Poor sleep
- Fasting less or more than your body needs
- Injuries or infections
- Intolerance to foods, supplements, or medications
- Environmental toxins and/or allergens
Interestingly, researchers believe that kisspetin may be particularly sensitive to nutritional stressors. In general, your diet can pack a powerful punch when it comes to influencing hormone balance, ovulation, and fertility - for better or worse.
Managing Stress for Hormone Balance

What are your biggest sources of stress? Below we’ll take a closer look at a few different sources of stress mentioned above and what you can do to manage them better.
1) Psychosocial or Psychological Stress
Psychosocial or psychological stress is stress surrounding social life and situations evoking an emotional response. These can include:
- A fear of being excluded
- Social performance anxiety
- Interpersonal conflicts
- A fear of being negatively judged by others
- Experiencing trauma, abuse, or violence
So what can you do to reduce psychological stress?
Tips to Kick the Stress
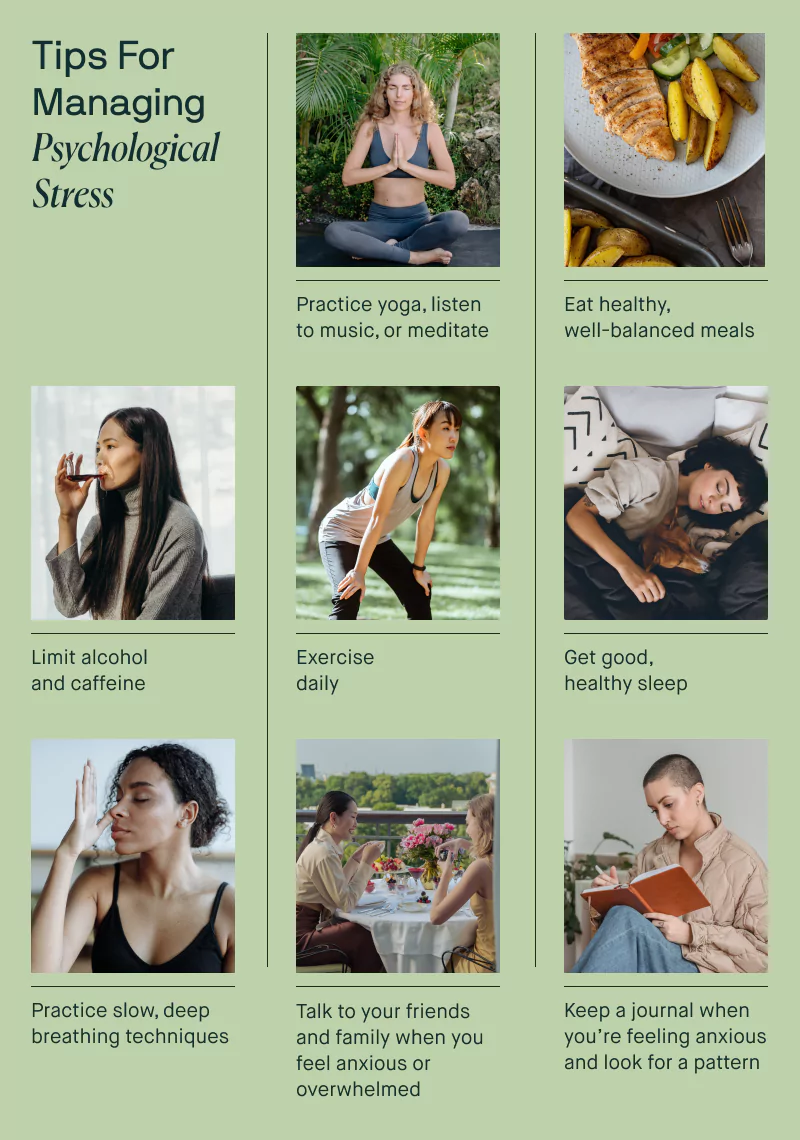
Mindfulness or Meditation
Mindfulness is a type of wellness practice that involves breathing exercises, guided imagery, and other meditative techniques to cultivate a sense of feeling present and in the moment.
Meditation exercises can help relax the mind and body. They may also help reduce stress and anxiety, and improve general well-being.
Therapy and Social Support
Therapy can also be a useful treatment for anxiety and stress that can be personalized for your specific needs. Cognitive Behavioral Therapy (CBT), for example, teaches people that they can change their way of thinking, behaving, and reacting to situations.
The Anxiety and Depression Association of America has even more tips for managing psychological stress, such as practicing yoga, eating balanced meals, and getting regular exercise.
2) Nutritional Imbalances
Most people may not automatically think of nutritional imbalances as stressors, but that’s exactly what they are! It’s stressful for the body to not have what it needs nutritionally to do the physical work of everyday life.
On the opposite end of the spectrum, excessive intake of nutrients beyond what you need is also a stressful situation for your body. Nutritional imbalances can lead to changes in hormones and menstrual irregularities.
PCOS, or polycystic ovary syndrome, is associated with insulin resistance, excess body fat, and hormonal irregularities that can negatively affect the menstrual cycle. However, a low-GI diet has been shown to positively impact these parameters in people with PCOS.
Too much or too little fasting may also negatively impact hormonal health. A study looking at lean women and fasting determined that changes in neuroendocrine function, anovulation, and a lengthened follicular phase occurred after fasting. This may suggest that lean women can be more vulnerable to fasting stress than normal weight women.
Some preliminary studies suggest that strategic short-term fasting during the luteal phase may actually reduce menstrual symptoms. However, it’s important to work with a healthcare professional such as a gynecologist or a registered dietitian when exploring fasting approaches.
Tips to Kick the Stress

Your body is unique, and so are your nutritional needs. Working with a qualified nutrition professional can be very helpful in finding what works best for your body.At this time, researchers have found important connections between menstrual health and:
- Eating regular balanced meals
- Getting enough protein
- Getting adequate essential fatty acids
- Getting the right balance of vitamins and minerals
- Getting adequate fiber
- Minimizing alcohol
- Reducing caffeine
3) Too Much or Too Little Exercise
Regular physical activity is crucial for your body’s health. Both too little and too much exercise can act as stressors on the body in ways that may negatively impact hormones.
Over-training, especially when not adequately fueling, is associated with amenorrhea (the absence of menstruation) and other unhealthy metabolic changes in female athletes.
Appropriate and well-fueled exercise can be beneficial for sex hormones and menstrual function. Aerobic exercise may also reduce symptoms of PMS, but more research is needed to confirm these findings.
Tips to Kick the Stress

Again, it’s all about personalization. You should customize your exercise to your particular enjoyment level and physical ability.
It’s also important to make sure you are fueling well enough to support your physical activity. If in doubt, work with an expert to help you customize your fueling strategy to your workout and fitness goals.
If you’re new to exercise and haven’t been in the habit of regular exercise, check out our articles about glute and hamstring exercises and chest and shoulder workouts for beginners!
4) Poor Sleep

Studies show that diet can impact sleep, and that poor sleep can negatively affect your blood sugar. Sleep can also play an important role in the menstrual cycle.
The American Academy of Sleep Medicine discusses how delayed sleep phase syndrome, a condition in which your sleep pattern is delayed by two or more hours from a conventional sleep pattern, is associated with irregular menstrual cycles and PMS.
In this research, premenstrual problems like cramps and mood swings occurred in 69 percent of subjects with the syndrome, compared to 16.67 percent of the control group.
Another study also found that the menstrual cycle may affect one’s quality of sleep, though the finding was not deemed clinically significant. Interestingly, a poor diet seemed to increase the likelihood that someone would sleep poorly during menstruation.
Tips to Kick the Stress
To ensure you are getting a good, healthy night of sleep, the Centers for Disease Control and Prevention (CDC) recommends:
- A consistent sleep schedule. Opt for at least 7 hours a night, and try to go to bed and wake up at the same time every day.
- Be mindful of what, and when, you eat and drink. Try not to go to bed hungry, but avoid large meals within a few hours of bedtime. Limiting nicotine, caffeine and alcohol is advisable.
- Create a restful environment. Avoid screen time just before bed time, and keep your room dark, quiet, and at a comfortable temperature.
- Limit long naps during the day. If you do need a nap, don’t nap for more than an hour, and avoid napping late in the day.
Since sleep quality can also be influenced by diet and other stress factors, addressing any nutrient imbalances or other stress factors can go a long way in supporting sleep!
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.





