Is Adrenal Fatigue Real?

Key Takeaways
If you’ve experienced persistent low energy levels or chronic fatigue, you may have heard of something called “adrenal fatigue.” This term is also often applied to someone who might be experiencing some form of “burnout.”
But did you know that the existence of “adrenal fatigue” is not recognized as a formal diagnostic term by the medical community? Why is it that this condition is not recognized by experts as a medical diagnosis? And why is there so much controversy surrounding adrenal fatigue?
In this article, we’ll explore the details of adrenal fatigue and what else might be going on in the body to cause these symptoms.
What is Adrenal Fatigue?
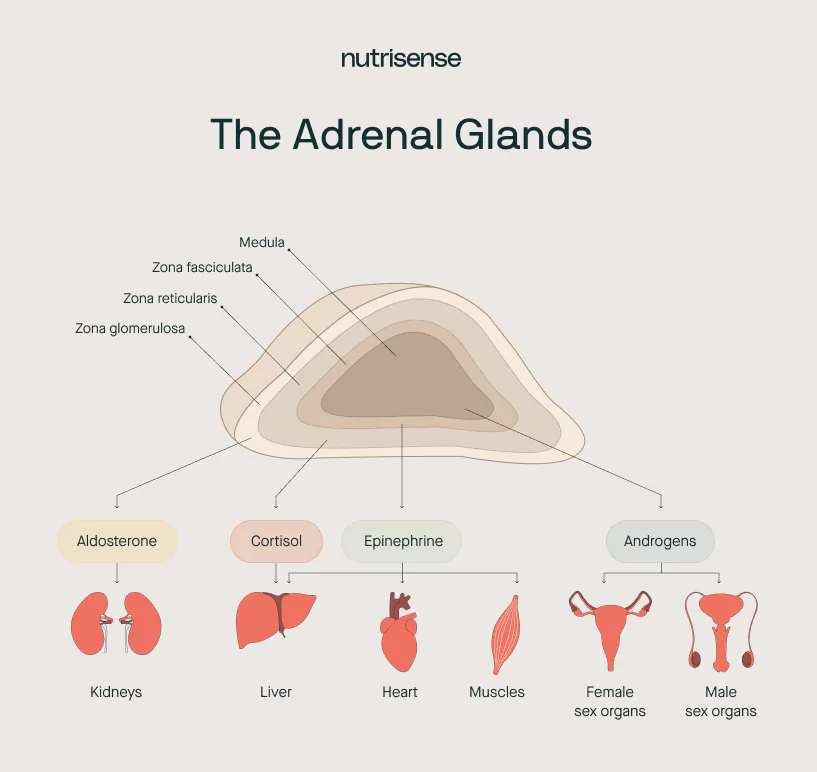
The adrenal glands are endocrine glands situated on top of the kidneys. The adrenals work in coordination with other endocrine glands, such as the pituitary gland to help your body respond to stress. These glands also control secretion of your primary stress hormone, cortisol, as well as adrenaline and other other steroid hormones.
The adrenals are but one part of the neuroendocrine or stress-response system. And while their function may be impaired during times of acute or even chronic stress, they may be only one part of a larger story of stress response unfolding.
Many consider “adrenal fatigue” a misnomer for a set of symptoms better identified by the CDC under the header of Chronic Fatigue Syndrome (CFS) or Myalgic Encephalomyelitis (ME). Others might consider it a lay term for generalized adrenal insufficiency such as Addison’s disease.
Is There a Test For Adrenal Fatigue?

The simple answer is no. Given that the term "adrenal fatigue" is not a recognized diagnostic label for a medical condition, testing doesn’t formally exist.
Assessing adrenal function and cortisol levels with blood tests, urine, or saliva in these cases is not a reliable diagnostic method. However, cortisol levels may be evaluated alongside other methods for diagnosing Cushing’s Syndrome or Addison’s Disease.
Several studies have looked for consistent biomarkers of “burnout” but findings were conflicting. However, for recognized conditions such as CFS/ME, the CDC does have some symptomatic criteria for diagnosis we’ll talk more about below.
Adrenal Fatigue or Chronic Fatigue Syndrome?
According to data from the Institute of Medicine (IOM), an estimated 836,000 to 2.5 million Americans suffer from CFS/ME and the vast majority of them have not been diagnosed.Some researchers have even suggested that the terms CFS/ME are inadequate to capture the true extent of the condition, instead proposing a new term: Systemic Exertion Intolerance Disease or SEID.
Either way, it may feel understandably confusing to navigate the conflicting opinions out there. Not only is the diagnosis of this condition difficult due to the variety of symptoms, but many of the symptoms can easily be attributed to other conditions.
What are the Symptoms of Adrenal Fatigue?
The symptoms typically associated with conditions such as CFS/ME may include:
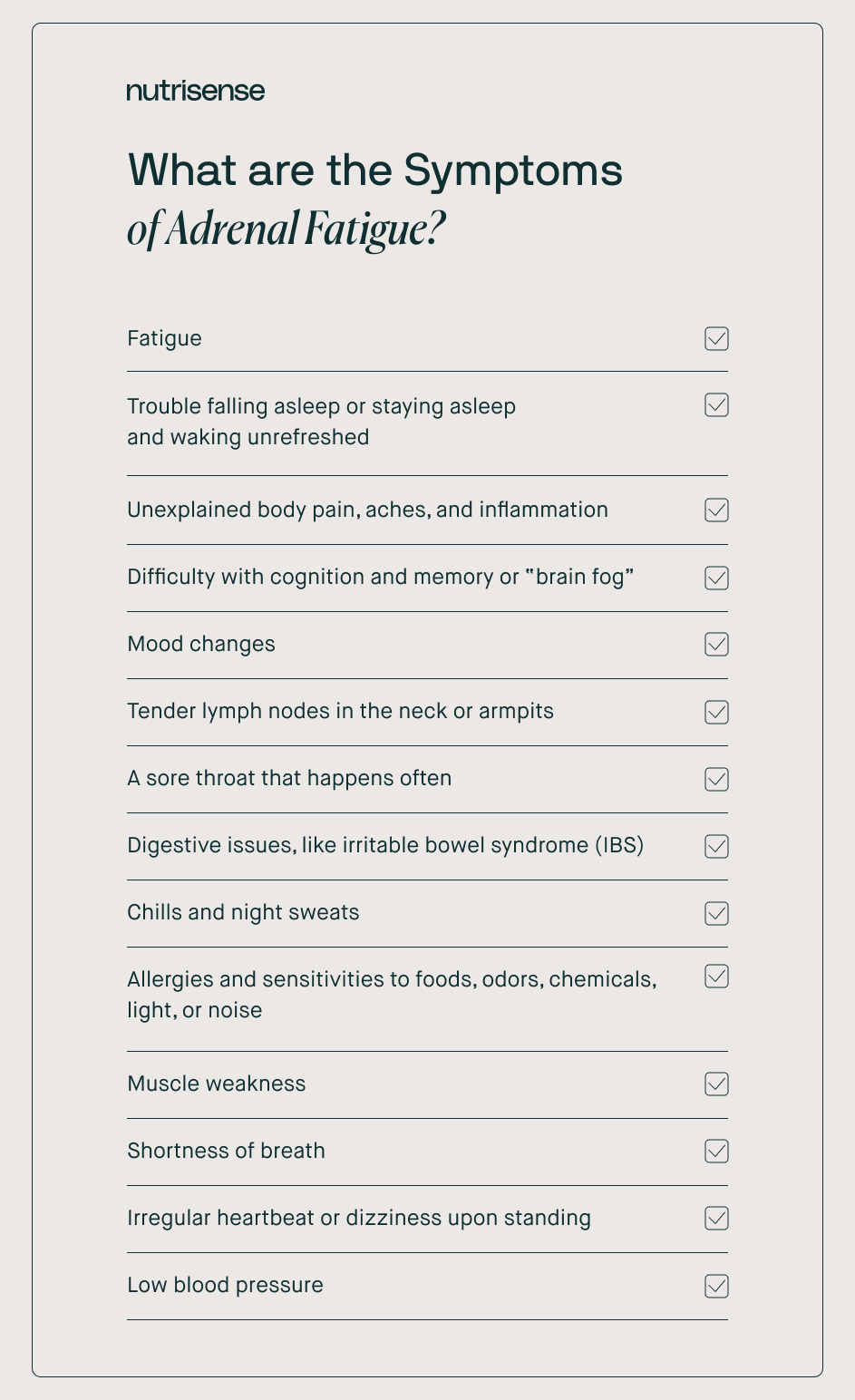
Symptoms may also worsen over time for someone and can exist along a continuum of moderate to truly debilitating. The CDC lists three core criteria or primary symptoms for diagnosing CFS/ME, including:
1) A Significant Loss Of Ability To Perform Daily Activities
People with CFS/ME often have fatigue that is worse than normal tiredness that can occur after doing a hard activity. The fatigue in CFS/ME often exists even without doing anything exceptionally difficult, and resting or sleeping may not make it better.
According to the CDC, a drop in activity level or tolerance along with fatigue must last six months or longer for a CFS/ME to be considered.
2) Post-Exertional Malaise (PEM)
PEM involves the worsening or flare-up of symptoms after a physical or mental stress trigger. This experience is commonly referred to as a "crash,” “relapse,” or “collapse.” It may take days, weeks, or longer to recover from a crash.
Crash triggers can be unpredictable, and can even cause you to be bed-bound for a period of time. A crash-triggering stressor for someone with CFS/ME will often be something that seems benign or unharmful to someone without this condition. We’ll talk more about triggers below.
3) Sleep Problems

People with CFS/ME may not feel refreshed or energized after a full night’s sleep. Problems with sleep apnea or insomnia, including falling asleep and staying asleep, are also common.
Other Symptoms
In addition to these three core criteria, the CDC also requires one of the following for diagnosis:
- Problems with thinking and memory. This can include trouble remembering things and a feeling of “brain fog.”
- Orthostatic intolerance. People with CFS/ME may be lightheaded, dizzy, weak, have blurred vision, or faint while standing or sitting up.
What Can Lead to Adrenal Fatigue Symptoms?
So, what is happening in cases where the body seems to be unable to tolerate or adapt to stress effectively? Though there is no firm consensus across the board regarding the precise mechanism, there are many evidence-based ideas.
Stress, the Neuroendocrine System, And Chronic Fatigue
A stressor is any type of pressure applied to your body that may knock it out of homeostasis (or equilibrium). What your body does to adapt to the stress is called a stress response. As we’ve mentioned in prior blogs on the effects of stress, any of the following may be considered stress by the body:
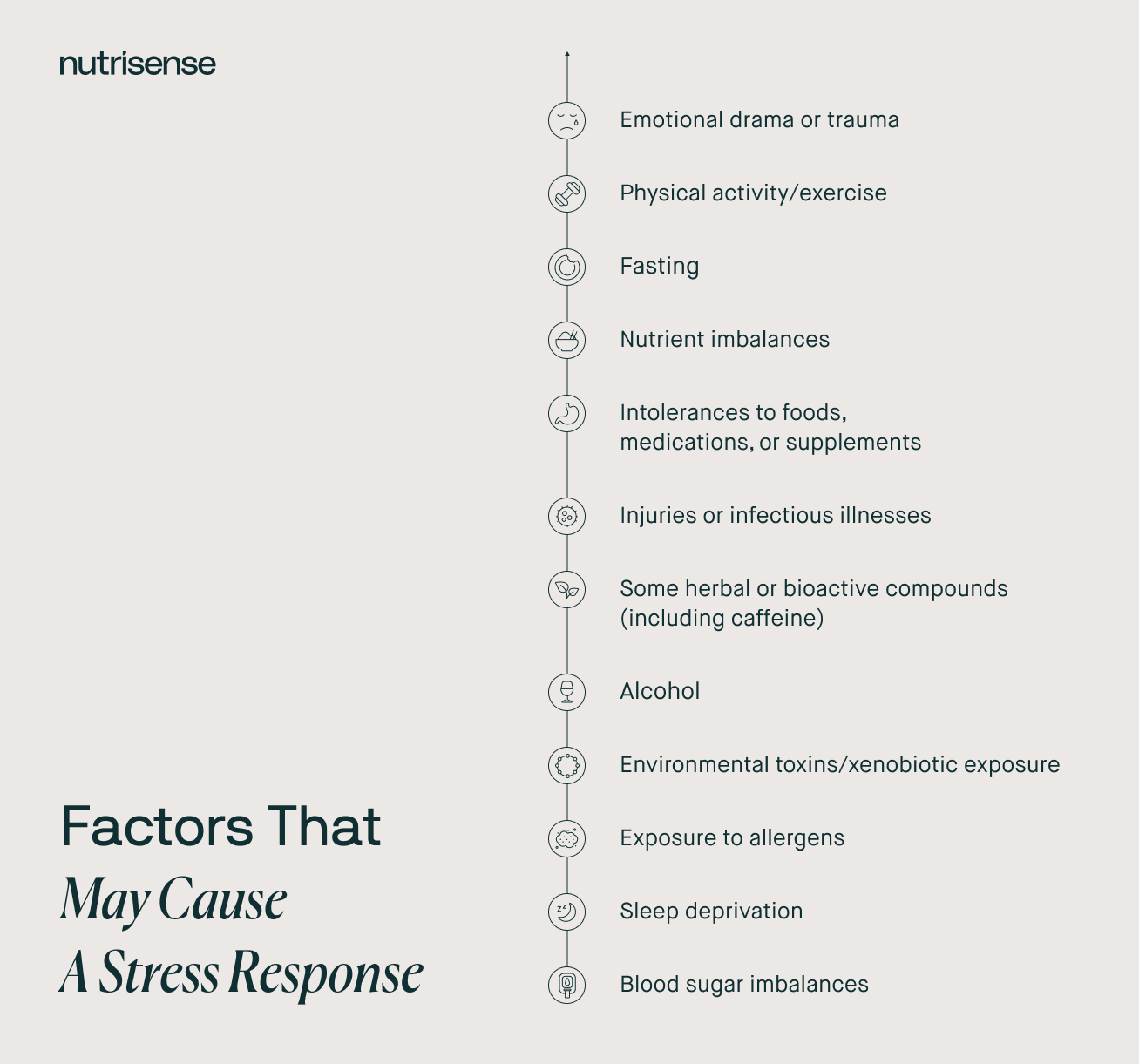
Many factors can also impact how our body interprets or copes with any of these stressors, such as age, sex, genetic predisposition, medical conditions, and other stressors.
The neuroendocrine system is your stress-response system. Some activities controlled or influenced by the different axes of this system are:
- Your digestion and absorption of food
- Your blood sugar regulation
- Your sleep/wake cycles
- Your menstrual cycles and reproductive health
- Your immune system function and inflammation
- Your mood
- Your body temperature, blood pressure, and heart rate
- Your exercise stamina and recovery
- Other hormonal levels
You might notice this list looks familiar! These areas are also the sites of common complaints and symptoms in CFS/ME we listed above. They are also common sites for symptoms of stress overload, or what is more formally referred to as allostatic overload.
With cases of chronic stress, researchers believe that certain symptoms might not be related to a state of “adrenal fatigue,” per se, but instead, a system-wide change in function as the body tries to adapt to the flood of incoming stressors and can’t quite keep up.
Allostatic Overload
Allostasis is the active process of maintaining homeostasis. Allostatic load is the cumulative burden of chronic stress on the body.
However, when stressors exceed the body’s ability to adapt or cope, something called allostatic overload can occur. Studies show that short-term stressors of different kinds may be beneficial. However, the same stress applied over longer periods of time may be very detrimental.
Chronic allostatic overload has been associated with a higher risk for a number of diseases and conditions, including:
- Cardiovascular disease
- Diabetes
- Some types of cancer
- Impaired immune function, including heightened autoimmune disease risk
- Digestive disorders
- Migraines
- Mental illnesses
- Weight changes, such as weight loss or weight gain
- Fatigue
Blood Sugar and Chronic Fatigue Syndrome

Some studies have suggested that CFS may be associated with metabolic syndrome and changes in glucose regulation, which can further worsen fatigue symptoms. Metabolic dysfunction related to altered ability to use fatty acids and amino acids as fuels is also seen in some research in CFS.
Other studies suggest that this dysfunction, along with other changes in the body’s ability to use glucose may make these individuals more prone to hypoglycemic episodes as well.
When blood sugar falls too low in hypoglycemia, this can act as its own independent stress on the body. Effectively managing blood sugar levels in those with CFS or similar conditions may therefore be an important component of therapy.
Is There a Treatment For Chronic Fatigue?
Perhaps one of the most important elements of managing CFS/ME or conditions of chronic allostatic overload is understanding crashes, triggers for crashes, and how each person’s response to stressors may be different.
Customizing a therapeutic approach in navigating crashes and crash triggers is best guided by a qualified medical professional with extensive experience. Some medical assessments and therapeutic approaches that may be guided by your medical provider, including qualified nutrition professional, might include:
- Any necessary blood work and other exams to rule out specific primary conditions with similar symptoms
- A customized dietary approach to meet your unique nutrient needs and identify any food or supplement intolerances
- A customized exercise program that includes appropriate levels of activity for your condition to avoid triggering crashes
- Appropriate adjustments of medications
- Emotional stress management techniques
- Social and mental health support
Can Supplements Help With Chronic Fatigue Syndrome?
So far, the research looking at the use of various supplements or generic diets in CFS or similar conditions has found insufficient evidence to support their use. Some doctors are also concerned that supplements or vitamins sold as a treatment for adrenal fatigue could lead to side effects that cause more harm than good.
One cautionary statement from The Endocrine Society says:
“If you take adrenal hormone supplements when you don’t need them, your adrenal glands may stop working and become unable to make the hormones you need when you are under physical stress. When these supplements are stopped, a person's adrenal glands can remain ‘asleep’ for months. People with this problem may be in danger of developing a life-threatening condition called adrenal crisis.”
As always, it’s best to proceed with any medication or supplement prescriptions or recommendations from a qualified healthcare professional.
Engage with Your Blood Glucose Levels with Nutrisense
Your blood sugar levels can significantly impact how your body feels and functions. That’s why stable blood glucose levels can be an important factor in supporting overall wellbeing.
With Nutrisense, you’ll be able to track your blood glucose levels over time using a CGM, so you can make lifestyle choices that support healthy living.
When you join the program, our team of credentialed dietitians and nutritionists are available for additional support and guidance to help you reach your goals.
Ready to take the first step? Start with our quiz to see how Nutrisense can support your health.
This article was written and published with permission by Heather Davis, MS, RDN, LDN.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Isra Bashiti is a registered dietitian nutritionist who grew up in Texas and graduated with a Master’s degree in Nutritional Sciences and Dietetics. She worked in the clinical setting for a few years as a Health Coach and Dietitian, focusing specifically on preventative health and community nutrition.


.webp)

