Is There A Connection Between Stress and Migraines?
.webp)
Key Takeaways
As anyone who suffers from migraines knows, the onset of debilitating migraine pain can have a significant impact on your quality of life. A migraine itself can be a stressful event, especially as you figure out how to accommodate this unwelcome guest into your day.
But could stress potentially be what triggers the arrival of your migraine or the condition itself? What impact could high stress levels be having on other areas of your health?
Read on to learn more about the connection between stress and migraine, migraine prevention, and what you may be able to do to bring relief when they occur.
Understanding Migraine

Migraine is a broad term that goes far beyond a typical headache. Considered a neurological disease, migraine can lead to a number of different symptoms and can affect each person in a different way depending on the type of migraine.
Common migraine triggers can include high levels of stress, certain lifestyle changes, not getting enough sleep, hormonal changes, certain foods, bright lights, and even changes in weather.
Though you may associate migraines with localized head pain or tension headache, other types of migraines such as abdominal migraines do exist and can bring painful abdominal symptoms and even cyclical vomiting.
According to neurology research, migraine is one of the leading causes of disability worldwide, impacting up to 25 percent of adults. The most common symptoms of migraine include:
- Head pain
- Sensitivity to light and sound
- Nausea
- Brain fog and dizziness
- Confusion
- Mood changes
- Fatigue
When it comes to migraine treatments, there are a number of different over-the-counter and prescription medications that may aid in reducing the symptoms. For some people experiencing chronic migraines, your doctor may prescribe a type of medication called triptans as a treatment option.
However, there are also a number of preventative treatment options that may also be effective in reducing the frequency of migraine and even prevent it from occurring altogether.
The 7 Types of Migraine
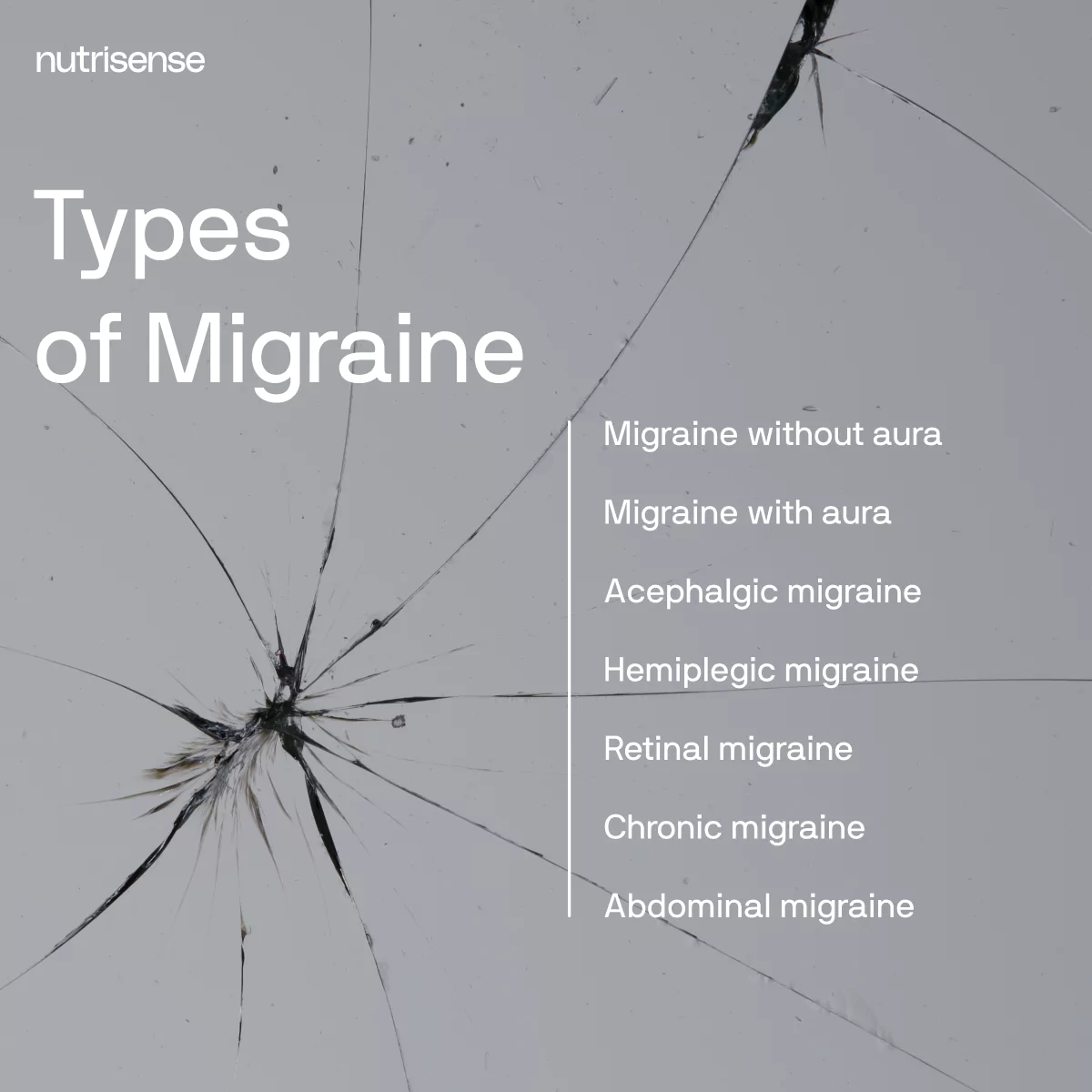
According to the headache classification committee of the International Headache Society and the American Migraine Foundation, migraines can be broken down into the following seven subtypes:
1) Migraine Without Aura
Migraine without aura is a recurrent pulsing and moderate to severe headache of four to 72 hours with a unilateral location. Some people may notice it is made worse by physical activity and associated with nausea and light and sound sensitivity.
2) Migraine With Aura
Migraine with aura has recurrent attacks lasting minutes. This may come with one or more of the following unilateral symptoms: visual, sensory, speech and language, motor, brainstem, and retinal, usually followed by headache and migraine symptoms.
3) Acephalgic Migraine
Acephalgic migraine is also sometimes known as a “silent migraine” or a migraine without headache. Even though there may not be an acute headache involved, the visual symptoms are identical to the episodes that are associated with a classic migraine aura.
4) Hemiplegic Migraine
Hemiplegic migraine is a rare subtype of migraine with aura. With this type of migraine, there is a presence of motor weakness and occasionally impairment in sensation or speech may also be seen.
5) Retinal Migraine

Retinal migraine is another rare form of migraine in which there may be temporary loss of vision in one eye. This is often accompanied or followed by a headache within 60 minutes of visual symptoms onset.
6) Chronic Migraine
Someone may be diagnosed with chronic migraine when they experience 15 or more days with headache pain per month for more than three months. To qualify as chronic migraine, at least eight of those headache days must have migraine symptoms.
7) Abdominal Migraine
More commonly diagnosed in children, abdominal migraine is central abdominal pain occurring in episodes alongside other features of migraine and associated with other syndromes such as cyclical vomiting and migraine limb pain.
Other Headache Types
Sometimes other types of headaches may be mistaken for migraine. These may include cervicogenic headache and cluster headaches.
Cervicogenic headache is most often triggered by an acute injury or disorder affecting the neck or cervical spine. Symptoms are usually limited to head and neck pain and sometimes include neck stiffness or changes in mobility.
Some researchers still debate whether or not cluster headaches and migraine are truly two distinct types of headaches. However, some of the key differentiating features between a migraine attack and cluster headache may include the duration of the headache, frequency, and the location of the pain.
Stress and Migraine
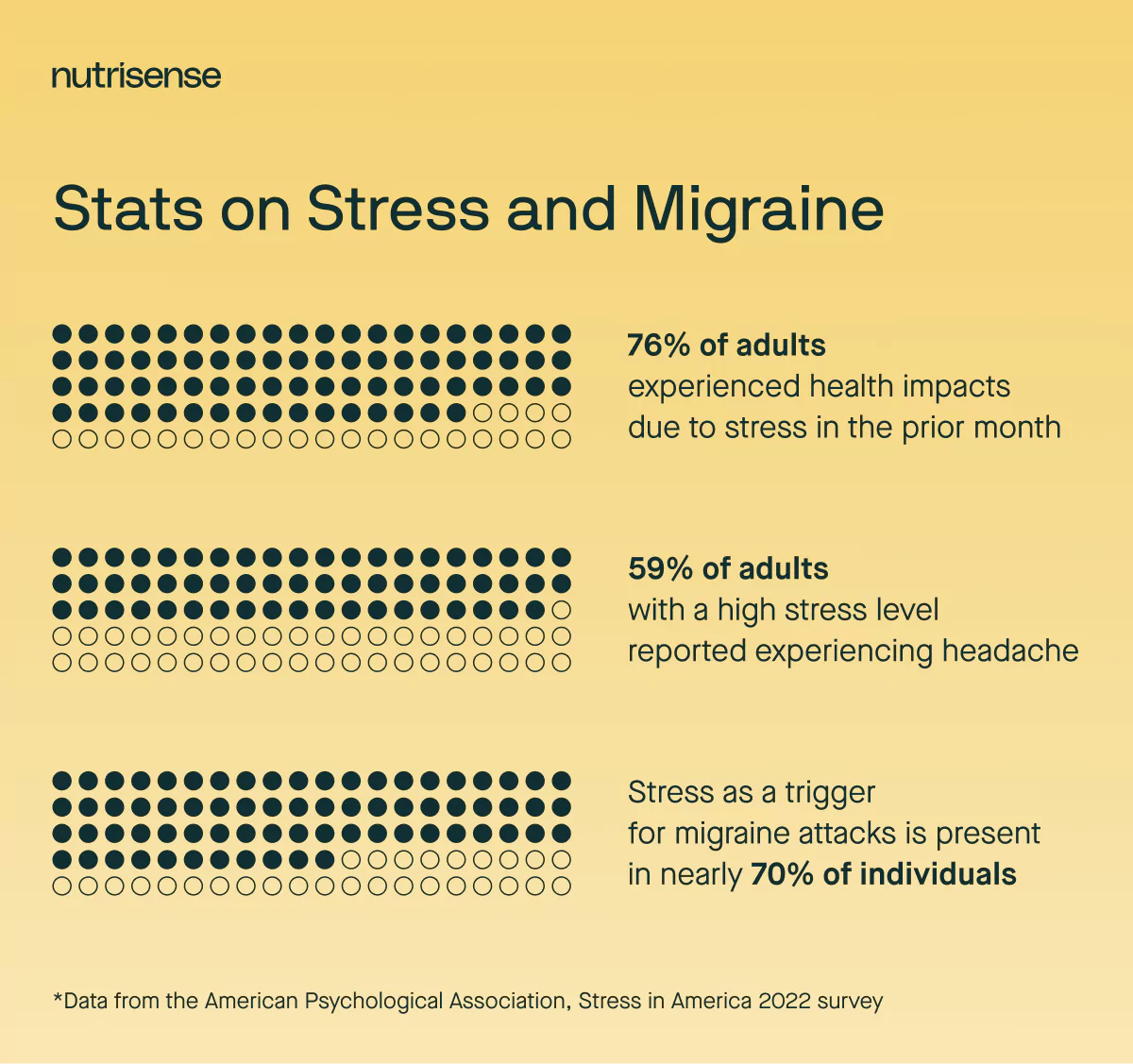
According to the American Psychological Association stress survey in 2022, 76 percent of adults said they have experienced health impacts due to stress in the prior month, including:
- Headache: 38%
- Fatigue: 35%
- Feeling nervous or anxious: 34%
- Feeling depressed or sad: 33%
Adults with a higher average stress level were more likely than those with a lower average stress level to report experiencing headache fatigue, feeling nervous or anxious, and feeling depressed or sad due to stress in the past month.
Some studies appear to suggest that stress causes migraine attacks in nearly 70 percent of individuals. So why is it that stress and migraine seem to be so connected?
A Closer Look at Stress
The research examining the connection between stress and migraine is still new and evolving. Some experts believe that the effects of repeated stress may lead to changes in brain networks.
This may in turn hinder how the brain responds to stress in ways that promote the development of the migraine condition. At the same time, chronic stress has been shown to increase risk for a great many health conditions and diseases beyond migraine such as cardiovascular disease, diabetes, cancer, sleep disorders, and even digestive disorders.
The type and amount of stress your body can tolerate before it begins to experience negative effects depends on many factors. These can be things like medical history, genetics or family history, and how many other stressors you are dealing with at the same time.
4 Tips and Techniques for Relieving Migraine Pain

While science may not yet know everything about how stress impacts migraine development or management for each case, there are many reasons to be assured that your efforts to reduce your perceived stress are worthwhile.
Wondering how you can begin to assess your daily stress levels and work to reduce your stressors? Here are four tips to get you started:
1) Identify Your Nutrition Stressors
Dietary and nutritional factors are often some of the most influential and yet overlooked sources of stress. Avoiding nutrient deficiencies and excesses is important, as is ensuring your meal timing and eating window are appropriate for meeting your needs.
Additionally, there are specific foods or substances that may be triggering for some, including alcohol and caffeine. Dose and frequency of intake may also impact migraine patterns for some people.
Glucose and Migraine

What about your blood sugar? Interestingly, glucose levels do appear to play a role in migraine triggers for some people.
Research shows that lower blood glucose levels can trigger or worsen migraine attacks. According to the same research, fasting or skipping meals is also one of the most well-known and frequently reported migraine triggers.
Other clinical studies have shown that sucrose-induced reactive hypoglycemia, especially when occurring after a meal, could also trigger migraine. More dramatic glucose fluctuations and dips in glucose levels may therefore be something to look out for.
Gut Health and Migraine
If you struggle with digestive issues as well as migraine headaches, you might find relief in addressing your diet from a gut health perspective. Various studies have shown a significant link between irritable bowel syndrome (IBS) and migraine, where those with IBS had a 60 percent higher risk of migraine than people without IBS.
Working with a qualified nutrition professional may be helpful. Seeking support from a registered dietitian (RD/RDN) or certified nutrition specialist (CNS) specializing in gut health can allow you to find ways of customizing your diet to better support gut health.
2) Assess Your Exercise Tolerance

For some people, certain types and amounts of exercise may trigger migraine. However, for some people, migraine can become a major barrier for regular exercise. As a result, lower levels of physical exercise may then worsen the severity and frequency of migraine attacks.
Considering this, some experts have suggested that a slower adaptation or conditioning approach to exercise may be the best approach, including things like stretching routines and yoga. It’s also important to ensure exercise is properly fueled with adequate nutrition to avoid drops in blood sugar that may act as triggers for migraine.
3) Support Sleep Hygiene
Inadequate amounts of sleep or regular poor quality sleep can be a big stress on your body and lead to high cortisol levels. That’s why it’s important to do what you can to support healthy sleep patterns.
Not only does your diet have the potential to impact your sleep, but your daily routines, especially your nighttime routines, may affect it as well. Some studies report that poor quality sleep may increase the risk of migraine nearly four times.
4) De-Stress Your Environment

Taking stock of your psychosocial stressors can help you evaluate whether or not these are weighing heavily for you in your daily life. Carving out self-care time in the midst of a busy schedule or stressful situations might feel difficult, but setting boundaries for self-care takes practice. Don’t give up!
You can try implementing some relaxation techniques such as meditation, breathing exercises, or journaling into your routine to help with stress management. For some people, working with a healthcare professional specializing in cognitive behavioral therapy may also be helpful for reducing stress levels.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Jordyn has a bachelor’s degree in biology, a graduate degree in Human Nutrition and completed a dietetic internship at the Memphis VA. She's a dietitian at Nutrisense, and has experience working as a clinical dietitian at a VA medical center specializing in oncology and at the Mayo Clinic, working with a wide range of patients ranging from neonates in the NICU to adult ICU.




