Living with Autoimmune Conditions: Multiple Sclerosis

Key Takeaways
Living with an autoimmune disease isn’t easy. Like most chronic conditions, it can affect various aspects of your daily life. According to the National Institutes of Health, many Americans live with these conditions—up to 23.5 million. The same report also found that they disproportionately affect women and that (for unknown reasons) their prevalence is rising.

Autoimmune diseases occur when your immune system begins to attack your body's organs, tissues, and cells. It can be because of genetics or other underlying causes. From type 1 diabetes to Graves’ disease, Rheumatoid arthritis to Celiac disease, they can all significantly impact your quality of life.
Because autoimmune diseases affect everything from blood glucose levels and thyroid glands to insulin levels and obesity, it’s important to understand the specifics of a few common ones.
We’ve already talked about how autoimmune diseases affect your wellbeing and what it's like living with Hashimoto’s and Graves' disease. Since March is Multiple Sclerosis Awareness Month, we’re going to focus on what multiple sclerosis (MS) is, the different types, symptoms, and what managing and treating MS can look like for those who suffer from the condition. Read on to find out more.
What is Multiple Sclerosis?
Multiple sclerosis is a condition (typically diagnosed by a neurologist specializing in MS treatment) that affects your brain and spinal cord. Your brain and spinal cord make up your central nervous systems, and these central nervous systems control almost everything you do. So, it’s not surprising that the worsening of this condition can affect every aspect of your wellbeing, from bladder control to your vision.
Multiple sclerosis damages the Myelin sheath, the material that surrounds and protects your nerve cells. When this damage occurs, it blocks messages between your brain and body.
Presently, there is no known cause of multiple sclerosis, and there’s some debate over whether it’s even an autoimmune disease. We’re including it in this series since, like other autoimmune diseases, it can affect your immune system, leading it to destroy the myelin sheath that protects nerve fibers in your brain and spinal cord. As with many immune system conditions, most types of multiple sclerosis are more prevalent in women than men.
Are There Different Types of MS?

There are four different types of MS, each slightly different. They include:
1. Clinically isolated syndrome (CIS): This has the same symptoms of multiple sclerosis but occurs as a single, isolated incident. It’s one of the first signs that you may have MS. Still, healthcare providers usually wait till you’ve had two or more CIS episodes before an MS diagnosis.
2. Relapsing-remitting MS (RRMS): This is the most common type of MS and the first stage of disease progression for some. With RRMS, you have flare-ups or attacks called relapses, then recovery time with few or no symptoms. The time of the flare-up, remission, and between each relapse varies from person to person.
3. Secondary progressive MS (SPMS): If you have multiple episodes of RRMS over 10 or 20 years, you can develop a type known as secondary progressive multiple sclerosis. It can be challenging to diagnose, so healthcare providers usually wait for months before they do so. With this disease progression, you may have worsening symptoms that affect your daily life and limit mobility.
4. Primary progressive MS (PPMS): PPMS is a rare type of MS. The primary problem is nerve damage and lesions that form across damaged nerves in your brain and spinal cord. It isn’t easy to diagnose, and, unlike most types of MS, it may affect men more than women.
A Note on Radiologically Isolated Syndrome
While this is not technically part of multiple sclerosis, it’s important to understand the connection. Radiologically isolated syndrome, or RIS, is a neurological condition related to the central nervous system.
Healthcare providers usually spot this during MRIs. An MRI of your brain or spinal cord (or both) will reveal white matter lesions that do not indicate any other condition. According to research, RIS can increase the risk of developing MS within ten years for many people. While research is ongoing, it’s something to keep an eye on.
What are the Common Symptoms of Multiple Sclerosis?
The symptoms associated with multiple sclerosis vary. Some symptoms depend on how much damage your nerve fibers have and which nerves in your body are affected. Some cases allow people to continue their day-to-day lives with good MS symptom management.
But the disease progression can be more severe for others, affecting their quality of life. Here are some common symptoms of MS to be aware of:
Vision Problems

One of the first, most recognizable symptoms of multiple sclerosis is a problem with your vision. There are various ways that these symptoms display themselves. Sometimes, vision problems come and go when you have multiple sclerosis.
Occasionally, they can even resolve themselves. These issues can include diplopia (double vision), optic neuritis (pain and blurriness), nystagmus (involuntary eye movement), or (rarely) blindness.
Fatigue
Another common symptom of MS is fatigue, which approximately 80 percent of patients report feeling.
Difficulty Walking or Running

Difficulty walking or running is often found in multiple sclerosis patients. It's due to side effects of the condition like weakness, loss of balance, and fatigue. Physical therapy and medication can sometimes help.
Dysesthesia
Dysesthesia is when you feel like your torso is being squeezed, but it isn't. Patients with MS may experience this chronic pain most often, and it's usually caused by nerve damage.
Spasticity
Spasticity is when you feel stiff and experience muscle spasms. It’s most common in the legs of people who have multiple sclerosis.
Weakness
MS patients often experience muscle weakness, which usually results from the disuse of muscular tissue due to nerve damage. Rehabilitation and mobility aids can sometimes help.
Numbness
Numbness is another common side effect of multiple sclerosis. It’s usually found in the face and extremities and is sometimes the first symptom among multiple sclerosis patients.
Detecting and Diagnosing Multiple Sclerosis

Detecting multiple sclerosis is challenging, mainly because there are no tests specifically to diagnose the condition. When doctors diagnose multiple sclerosis, they often base it on symptoms their patient may be feeling or by ruling out other conditions with similar symptoms.
The diagnosis of multiple sclerosis may take a great deal of time and is sometimes misdiagnosed in the early stages. If your doctor thinks you may have multiple sclerosis, they may suggest the following tests:
Blood Tests: Blood tests are the first test recommended by most doctors. They check for biomarkers linked to the disease and, while they're just the first step, can help narrow down the diagnosis.
MRIs: MRIs, or magnetic resonance imaging, are tests used to reveal lesions on your spinal cord and brain. Your doctor may give you an intravenous injection of contrast materials to highlight lesions and your brain and spine. It will indicate whether you have multiple sclerosis and if it is active.
Spinal Tap: If your doctor thinks there’s a possibility you have multiple sclerosis, they may suggest that you get a spinal tap or lumbar puncture. It's when your doctor will remove a small sample of cerebrospinal fluid from your spinal cord. This sample is then analyzed in a laboratory to show antibody abnormalities.
Evoked Potential Testing: Evoked potential tests record electrical signals responding to stimuli in your nervous system. These tests use visual stimuli and electro stimuli of different types—for example, you watch a visual pattern, and the test tracks your eye movements. Others send tiny electrical impulses into the nerves in your legs or arms. Your doctor will then measure how quickly you process the information in your nerve pathways.
How to Treat Multiple Sclerosis

Presently, there is no known cure for multiple sclerosis. Treatments focus on how to manage symptoms and help patients return to as regular a routine as possible. If caught early enough and treated correctly, some patients with multiple sclerosis may only experience mild symptoms.
Some doctors may recommend medication to deal with your symptoms like anti-depressants, muscle relaxants, and physical therapies.
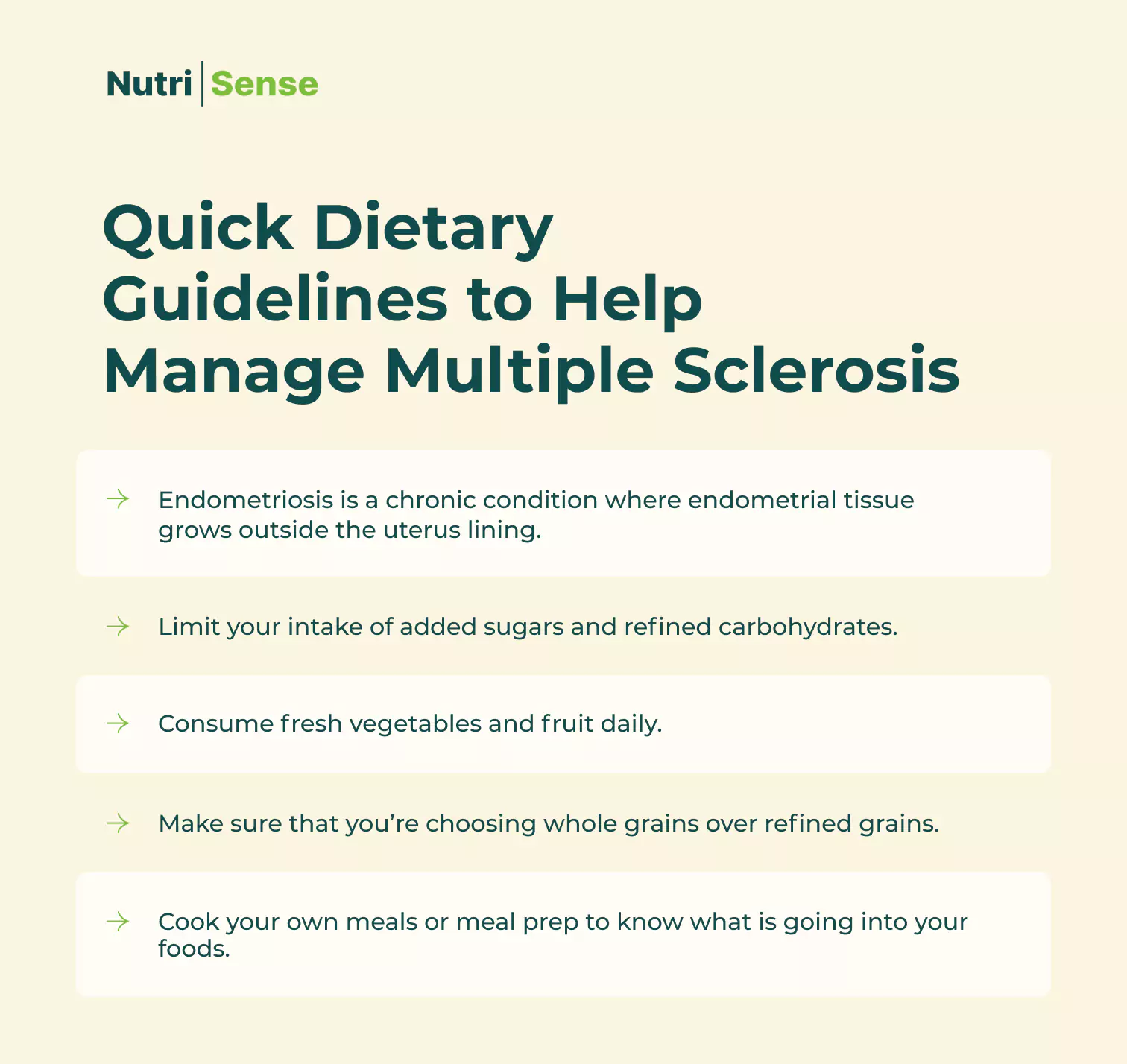
If you have multiple sclerosis, your doctor will probably ask you to change your lifestyle. These include regular physical activity, a healthy diet according to your body‘s needs, preventing overheating, and managing stress.
Many nutrient-rich foods can also help you strengthen your immune system and manage the symptoms of multiple sclerosis. Remember, it’s best to work with a doctor or dietitian before making any significant changes to your diet. Working with a professional is the best way to begin working with your body to alleviate symptoms healthily.
Monitoring Your Blood Sugar with Multiple Sclerosis
Research shows there is no one specific diet to follow if you have multiple sclerosis. While there may be a lack of guidelines regarding a particular diet, developing healthy dietary and lifestyle habits is key to managing your symptoms. So, also focus on limiting sugar intake and tracking and monitoring your glucose levels. Balanced blood sugar levels can help your body deal with the symptoms that you may be experiencing due to multiple sclerosis.
Finding Support to Manage Multiple Sclerosis

Managing an autoimmune disease can be challenging, but you don’t have to do it alone. Caregivers can be helpful, and having family or friends as pillars of support is invaluable. But often, it’s helpful to speak with people who know and understand first-hand what you’re going through.
It can be a good idea to find an MS support group. Support groups can help you find new ways (and motivation) to ensure you’re living well. They're also a good resource for symptom management and can be a sounding board when you want to discuss new treatments. And, perhaps most importantly, speaking with people who are going through similar challenges as you are can be good for your mental health.
The National Multiple Sclerosis Society has excellent resources for those with this condition. You can find mental health and support groups, MS treatments, financial support, legal resources, and much more.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Cheri is a registered dietitian and Health Co-Ordinator Product Development at Nutrisense, with a Master's degree from the University of Utah in Integrative Physiology and Nutrition. She has a strong interest in functional and integrative nutrition and emphasizes the importance of exploring and using your own body (symptoms, energy, mood, labs, CGM data) to find what your personal optimal is.


.webp)

