How CGMs Can Improve Your Fitness Performance

Key Takeaways
It’s safe to say athletes take their training routines seriously. So seriously that they’re eager to utilize any tools, from gels and supplements to smartwatches and wearable health tech, to improve performance.
Since intensive training requires continuous testing and monitoring, many people who exercise regularly often opt for periodic blood testing to check for deficiencies or other health markers. These tests typically include ones for glucose concentration and fasting blood sugar.
A fasting blood sugar measures blood sugar at a single point in time and can be used to diagnose prediabetes and diabetes. But it does not allow people to measure and track their glucose values continually. Something that fills that gap is a continuous glucose monitor, once worn primarily by people with diabetes but quickly becoming a wearable preventive health device for healthy people.
It can be one of the best ways for anyone participating in an endurance sport to track glucose levels continuously. The device has only recently become popular among other populations, including those interested in endurance exercise and endurance sports. So, the research on CGM device use among sports enthusiasts without type 1 diabetes is limited.
Athletes with type 1 diabetes have used CGM technology for years to help plan training, nutrition and make more critical decisions like how much insulin they need. An athlete without type 1 diabetes may not need to make decisions about insulin, but they can still use this device to help them gain important information about their training and fueling strategies.
Why is Continuous Glucose Monitoring Effective for Sports Enthusiasts?

You likely know of fasting blood glucose since this is a pretty standard blood test. Blood glucose, also known as blood sugar, is a type of sugar that your body uses for various processes. When you’re active, your body uses glucose to fuel muscles.
Glucose is also an important fuel source for your heart, kidneys, nerve cells, and white blood cells. Glucose comes from carbohydrate foods such as grains, starchy foods, milk products, fruits, and sugary foods such as candies and soda.
Many carbohydrate foods contain many glucose or sugar molecules linked together, which enzymes in your gut then have to unlink. Glucose is then absorbed and goes into the bloodstream. When you eat carbohydrates throughout the day, your body uses glucose as fuel.
The rest is stored as liver and muscle glycogen (glucose storage). However, if you exceed the capacity of the glycogen deposits, the glucose remains in the blood until it can be stored as fat, which leads to high blood glucose levels.
Most people use carbs as the primary source of energy before their training. Still, they also consume carbs after the exercise to restore glycogen deposits. The number of carbohydrates people consume are ususally based on estimations of energy and macronutrient needs and subjective measurements of how they feel during and after the training session. But a glucose monitoring system can help here.
It’s no surprise that people who exercise frequently flock to tools like the continuous glucose monitor (CGM) to see how their training and food intake impact their blood glucose levels in real-time. It allows them to make better decisions regarding their carbohydrate intake around training to maximize performance without compromising their health.
{{rich-text-cta-3="/style-guide"}}
Continuous Glucose Monitoring Is Becoming Increasingly Popular with Sports and Fitness Enthusiasts

Glucose control was once something only people who already had diabetes needed to monitor. But since monitoring your glucose data and glucose trends can be an effective preventive health measure, tools to monitor and track your blood glucose are becoming increasingly popular.
One of these tools is the CGM device, traditionally used by people with diabetes to avoid health complications and monitor their glucose levels. People with diabetes cannot produce insulin (type 1 diabetes) and/or cannot use insulin properly (type-2 diabetes).
The body uses the hormone insulin to allow glucose to move into the cells. If your body cannot produce or use insulin properly, you can experience high glucose levels (hyperglycemia). So, people with diabetes can use the CGM to monitor their glucose levels and make decisions (regarding food or medication) that help minimize the risk of high blood sugar.
What exactly is a CGM device and what are the benefits of using a CGM device? Simply put, it’s a small device attached to the skin (usually your upper arm), with a tiny flexible sensor that goes under the skin to detect blood glucose. While sensor lifetimes differ, they typically can be used for two weeks continually and measure glucose levels every one to fifteen minutes (depending on the device).
This continuous recording provides valuable information on glucose trends and fluctuations. The app connected to the device shows blood glucose levels in real-time. The CGM device allows everyone, including sports enthusiasts, to make diet and activity choices to improve glucose levels.
Constantly high blood glucose levels among those with diabetes can increase the risk of stroke, dementia, and kidney and nerve failure. However, evidence shows that elevated blood glucose even in someone without diabetes can lead to a higher risk of cancer, cardiovascular disease, inflammation, blood vessel damage, and diabetes.
Many runners and swimmers consume a higher carbohydrate diet to support their training. But for some people, this can lead to higher blood sugar levels. In addition, the intensity or duration of their exercise can cause glucose to rise or fall during training.
Seeing the changes in glucose can help provide valuable information about what they should be eating pre, during, and post-exercise. For some people who experience a release of adrenaline during training or racing, it can cause a significant increase in glucose or hyperglycemia.
Other considerations for a larger glucose spike during training could be due to the meal consumed prior to exercise or the release of glucose due to rapid glycogen breakdown during higher intensity training. It is possible that several of these factors may be involved. This may be another good reason to monitor blood glucose levels.
How Endurance Athletes Benefit from Monitoring their Blood Glucose

Many people in endurance sports follow a strict diet with high levels of carbohydrates that are meant to refill glycogen stores and improve energy levels and performance. In some cases, this can positively impact their lifestyle. Unfortunately, there are cases in which the athlete can have a low tolerance for carbs, leading to significantly higher sugar levels in the blood.
High-intensity physical training can release hormones, including adrenaline (epinephrine), causing a rise in blood sugar. The effect of these hormones on increasing the release of glucose from glycogen in the liver can be even more significant if you don’t eat before training.
However, if you have a history of high sugar levels, adrenaline can cause glucose levels to increase to very high levels, leading to an increased risk of cardiovascular disease. Glucose spikes above 180 can cause vascular damage so it is advised to keep glucose levels below 180 during exercise to avoid any risk.
Keeping track of glucose levels can improve the quality of life for a fitness enthusiast. Having a positive impact on performance and energy levels is just one of the many benefits of glucose monitoring through a CGM.
According to sports medicine researcher Dr. Andrew Jagim:
"[A CGM] could certainly be a valuable tool to use to get that feedback that you don't normally get when it comes to different feeding strategies and what may work for some, or how we can dial in some of the timing recommendations. It’s such a unique opportunity to have that little piece of metabolic data that can tell us many interesting things."
Endurance athletes may also be training for long periods, often hours at a time. If they do not fuel appropriately before and during training, they can risk low blood sugar. They can even experience hypoglycemia, in which their glucose levels can become too low which may lead to bonking or feeling a noticeable drop in energy levels and decrease in performance. Using the CGM, an athlete can monitor for dips in glucose or decreases in glucose during training and plan their fueling strategy accordingly.
CGMs can also help people with glycemic variability. Glycemic variability is a metric used to assess glucose fluctuations and, in most cases, will improve with exercise. However, if they're are engaging in a high-intensity workout in which their glucose is going very high or long-duration low-intensity exercise in which their glucose may be going low, they may see an increase in their glycemic variability.
A greater degree of glycemic variability is associated with an increased risk of oxidative stress and endothelial dysfunction (cells that line our blood vessels).
How Glucose Monitoring Maximizes Athletic Performance

Glucose monitoring can help maximize athletic performance for various reasons. For one, it’s an easier, less invasive method than other types of glucose measurements. Before CGM technology, if an athlete wanted to measure blood glucose, they would have to use a finger-prick device (glucometer). It allows you to measure glucose at one point and involves pricking the finger and then measuring the glucose in a drop of blood.
It’s an effective tool for some purposes, but it does not allow for the continuous measurement of glucose and is not practical during training because they would have to stop their activity to take the measurement.
The CGM, on the other hand, allows for continuous glucose measurement, is less invasive, and allows them to measure glucose during training without having to stop and take measurements. So, it’s no surprise they’re increasingly popular among everyone, from amateur to professional endurance athletes.
Some CGM devices are connected to Bluetooth, allowing the data to auto-populate. Others need to be scanned for the data to populate in the app. Using the CGM is becoming the most popular way for sports enthusiasts to keep track of their glucose levels.
In addition, there is evidence that CGM devices are accurate during intense training. Although there is limited research at this point, there is some evidence that the CGM can help increase performance and recovery.

It’s important to remember that everyone is different and will respond uniquely to carbohydrates. Dr. Jagim continues, "I think it's really important to approach a lot of sports nutrition guidance at an individual level. It's making sure that a specific person, wherever they are on that spectrum of insulin sensitivity, is getting the nutritional advice that works for them based on their health history and unique response.
"Then, if you have access to tools like a CGM, it can maybe make some more data-driven recommendations for that person to, again, kind of get them the best diet or dietary recommendations that they likely need, based on all that context and information about them."
Like anything, a CGM can be a valuable tool for some athletes, but not for all. It’s not a tool that controls blood sugar; but rather it can allow the person training, their doctor, and their dietitian to better understand their blood sugar and energy levels, even during a workout. It enables them to make diet and training decisions to help improve their performance and minimize any health risks associated with high or low blood sugar.
6 Reasons Your Glucose Might Spike During Exercise
With the help of a CGM device, a registered dietitian or nutritionist can plan a specific diet that meets all of the fitness enthusiast's energy needs. There are many situations in which a person will require the help of a licensed nutritionist, especially if it involves CGMs. So if you’re wondering how to better understand a few of the most common situations that you might meet along the CGM journey, here are a few of them explained:
1) Spikes in Blood Glucose During Zone 2 Training
Consider someone who uses a CGM and notices a considerable rise in blood glucose from low-intensity activities like biking, running, swimming, or yoga. In this case, they may benefit from minimizing their carbohydrate intake before exercising.
In the case of low-intensity exercise, blood sugar levels will not typically rise. In fact, someone who is training should notice the opposite in which blood sugar levels should decrease or remain steady as the body uses glucose and fat for energy.
During low-intensity or zone 2 cardio (approximately 60 percent or less of VO2 Max, or maximal oxygen consumption) most people will use more fat for fuel. As intensity levels rise there is a crossover in which the body starts to utilize more glucose and less fat.
This is why the person may notice their glucose values remain steady or decline slowly during this zone 2 training (depending on if they take in fuel during training). Large dips in glucose during low-intensity exercise and feeling of low energy or “bonking,” especially within the first 60 minutes of exercise, might be an indication the athlete is not fueling adequately or they are not efficiently burning fat and may need to improve metabolic flexibility.
The fitness enthusiast can use the information they get from the CGM to make changes to their fueling strategy with the goal to prevent bonking and improve their metabolic flexibility. A slight initial rise in glucose at the start of low-intensity activity may be okay, but a significant increase in glucose may indicate that they're consuming too many carbohydrates before exercise.
2) Higher Glucose Values During Intense Exercise

If a person sees a large spike during strength training or high-intensity interval training, it may indicate they're not getting enough fuel to support the movement. So the body responds by increasing hormones that release stored energy from the liver. In this case, they may benefit from having a well-balanced meal two to three hours before the exercise.
3) Glucose Spikes During Longer Training
Another example is if someone is experiencing extreme drops in glucose during a more extended training session like running or biking. It may be a sign they are not fueling properly before and during the workout.
In this case, a typical recommendation would be having a balanced meal with carbohydrate, protein, and small amounts of fat (macro amounts will differ depending on the person) about two to three hours prior and more consistent fueling during the activity with a specific target for carbohydrates per hour of training.
4) Dehydration-Related Spikes in Glucose

If someone sees a large spike in glucose despite fueling properly before exercising, it might be a sign of dehydration or a need for additional electrolytes. In this case, they would need to work on adequate hydration and electrolyte intake before, during, and after training.
5) Low-Carb Dips in Glucose

If a low-carb fitness enthusiast is experiencing extreme drops in glucose accompanied by low energy or poor performance, they can work on a fat adaptation and targeted carbohydrate intake plan that works within their goals.
6) Moderate-Intensity Training Dips in Blood Sugar
Sometimes, people may experience drops in blood sugar levels during moderate-intensity activities such as soccer, hockey, or lacrosse, combined with low energy levels. It means that glycogen (the storage form of glucose) is becoming depleted.
Since the body has a hard time relying on fat for fuel during moderate to high-intensity training, this can negatively impact performance.
The recommendation would be to have a pre-workout meal with carbohydrates and a post-workout meal balanced with carbs and protein to restore their glycogen deposits. They may also need to consider fueling during the session (likely at the midway point or half-time break in the game).
Sports Where Continuous Glucose Monitoring is Growing

CGM devices are most popular among people who struggle with high blood sugar levels, prediabetes, or even diabetes. Sports that cause the body to rely on glycogen as an energy source are the ones that often cause sugar spikes. You can find cycling, power sports, marathons, and dancing among these.
Many well-known athletes now wear CGM devices. For example, at the World Half Marathon Championships in Poland, Jake Smith wore a CGM device that registered his blood sugar fluctuations. The device showed a rapid decline in sugar levels during the training time for the race. His nutritionist advised eating more carbs during the day before the marathon to correct this. So he ate pasta, rice, chicken, vegetables, and fruits.
The following day, he had two bagels with Nutella and peanut butter in the morning. He ended up being the world’s best distance runner at the marathon. By keeping track of his glucose levels with the help of a CGM device, he corrected his glucose levels and performed his very best at the race.
Nutrisense Members Share Their CGM Experiences
See what these four Nutrisense members had to say about their experiences using a CGM in their respective sport.
Katie Kissane, MS, RD, and Nutrisense Nutrition Team Member

"When I wore the CGM I was able to see how my fueling was impacting my glucose levels. For instance, I noticed that doing a fasted run did not work well for me. My glucose levels would always spike up if I ran in the morning without eating first, but if I had a healthy breakfast and hydrated well before a run my levels would not spike and look more stable during the run.
I was also able to experiment with fueling during a few of my longer runs to determine how often I needed to consume carbs in order to prevent large drops in glucose and have more sustainable energy.”
— Katie Kissane MS, RD
Ian Hosek, Professional Endurance Coach and Athlete

Why Ian Loves the CGM
"I know how vital fueling for endurance events is and wanted to take my control to the next level. I wanted to try using a CGM for running to find out what works, what doesn’t, and how to maximize my performance when it matters most.
The application process was completely painless and super easy to follow the instructions. It was fascinating to see how my body reacts to different foods and how my glucose levels spike or don't spike.
I noticed that pre-meals, when I was low on energy, my glucose levels would reflect that. After some food and after they would normalize some, I would be back to normal and not feel sluggish anymore."
Anne Maher, Triathlete and 2:53 marathoner

Why Anne Loves the CGM
I have experienced firsthand (while competing in marathons and triathlons) how important it is for athletic performance to keep blood sugar stable. I thought that earing a CGM would provide valuable insight into my blood sugar levels during training to optimize performance in training and on race day.
I was amazed by how much stress impacted my blood sugar levels. On days that I experienced significant life stress, my blood sugar was significantly higher than when I had less stress.
One of the biggest takeaways for me was how stress impacts so much in our bodies, even blood sugar. I also did not realize that everyone's body responds uniquely to different carbohydrates and found it very helpful to see exactly which types of carbohydrates make my blood sugar "spike" and which keep my blood sugar in an optimal range.
I see a CGM as a valuable tool to see what is happening inside your body. It allows you to make tweaks to your daily habits to optimize your health. Seeing how your food choices and habits impact your body in real-time makes it easier to make changes and reach your goals."
Katie Olsen, Former Varsity Swimmer at Stanford and Director of Operations at Nutrisense
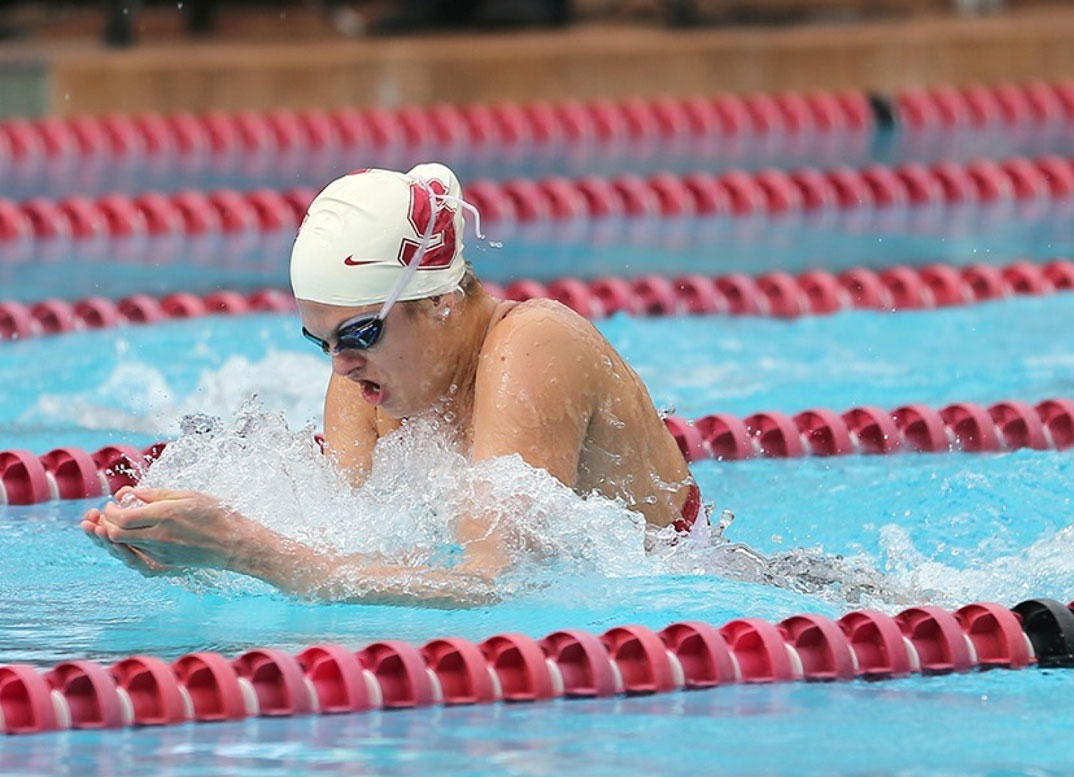
Why Katie Loves the CGM
“My fitness level has always been above average. I used to be a world-class competitive swimmer, so I’d say I was metabolically healthier than the average person (primarily due to my interest in nutrition and strict attention to my diet).
As an NCAA athlete with a rare chronic immune disorder, I got sick all the time, had to miss practice and class, and the U.S. healthcare system failed me. I wanted a solution. I had heard on various podcasts that metabolic health is crucial to a strong immune system, and the CGMs are a great way to measure that.
I was extra lucky to have Kara, our Director of Nutrition, as my RD during the program. My biggest learning was how eating protein before carbs or sugar greatly stunts the response. I had just moved to Paris, so the CGM made it crystal clear that my affinity for croissants and flat whites was not great for my health. I rarely eat carbs or sugar anymore without having an egg or other protein first.
The biggest (bad) food shockers were sweet potatoes (as a swimmer, we’re always told that these are the “best recovery foods!”) and sushi or corn products. I also learned so much about how stress impacts my immune health! Sure, diet, exercise, and sleep matter, but the stress was a blindspot that the CGM revealed for me.
We all have ideas and opinions about what is “healthy” for us, others, and society. And with so much information on CGMs, diet, and nutrition floating around the internet, it’s hard to “cut through the fat” and understand what matters for me, personally, what changes can have the highest impact on my goals, and what habits I have can sustain over time.
The continuous data and human support combo at Nutrisense helped me achieve a better result in three months than six years of reading books, articles, and listening to podcasts did."
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Amanda is a Nutrition Manager and Registered Dietitian, with a Masters in Dietetics from Stephen F. Austin State University. Originally from south GA, she got her undergrad degree from Texas Tech University. She worked at a hospital in Fort Worth, TX, for 4 years as a dietitian, counseling those living with HIV.



.png)
