A1C and Prediabetes: How Are They Connected?

Key Takeaways
An A1C test shows your average glucose over the past 2-3 months, with a level between 5.7% and 6.4% indicating prediabetes. This means glucose levels are higher than normal, presenting an important opportunity to make sustainable lifestyle changes that improve your metabolic health.
- Prediabetes is often caused by insulin resistance, a condition where the body's cells don't respond properly to insulin.
- Explore six healthy ways to help keep your A1C levels in a healthy range, including building a nutrient-rich meal plan.
- The Nutrisense program includes access to 1:1 insurance-covered video calls with a certified glucose expert and is currently available in the United States.
An A1C test shows your average glucose over the past 2-3 months, with a level between 5.7% and 6.4% indicating prediabetes. This means glucose levels are higher than normal, presenting an important opportunity to make sustainable lifestyle changes that improve your metabolic health.
- Prediabetes is often caused by insulin resistance, a condition where the body's cells don't respond properly to insulin.
- Explore six healthy ways to help keep your A1C levels in a healthy range, including building a nutrient-rich meal plan.
- The Nutrisense program includes access to 1:1 insurance-covered video calls with a certified glucose expert and is currently available in the United States.
Keeping your A1C in check
With the rising prevalence of prediabetes worldwide, understanding the connection between prediabetes and your glucose levels is increasingly important. A number of different factors can lead to an increased risk of this condition, and some people may experience few if any symptoms of prediabetes if they develop it.
Let’s explore the role of A1C levels in a prediabetes diagnosis, as well as healthy ways to keep your A1C levels in an optimal range and stay on top of your wellness.
What is an A1C test?
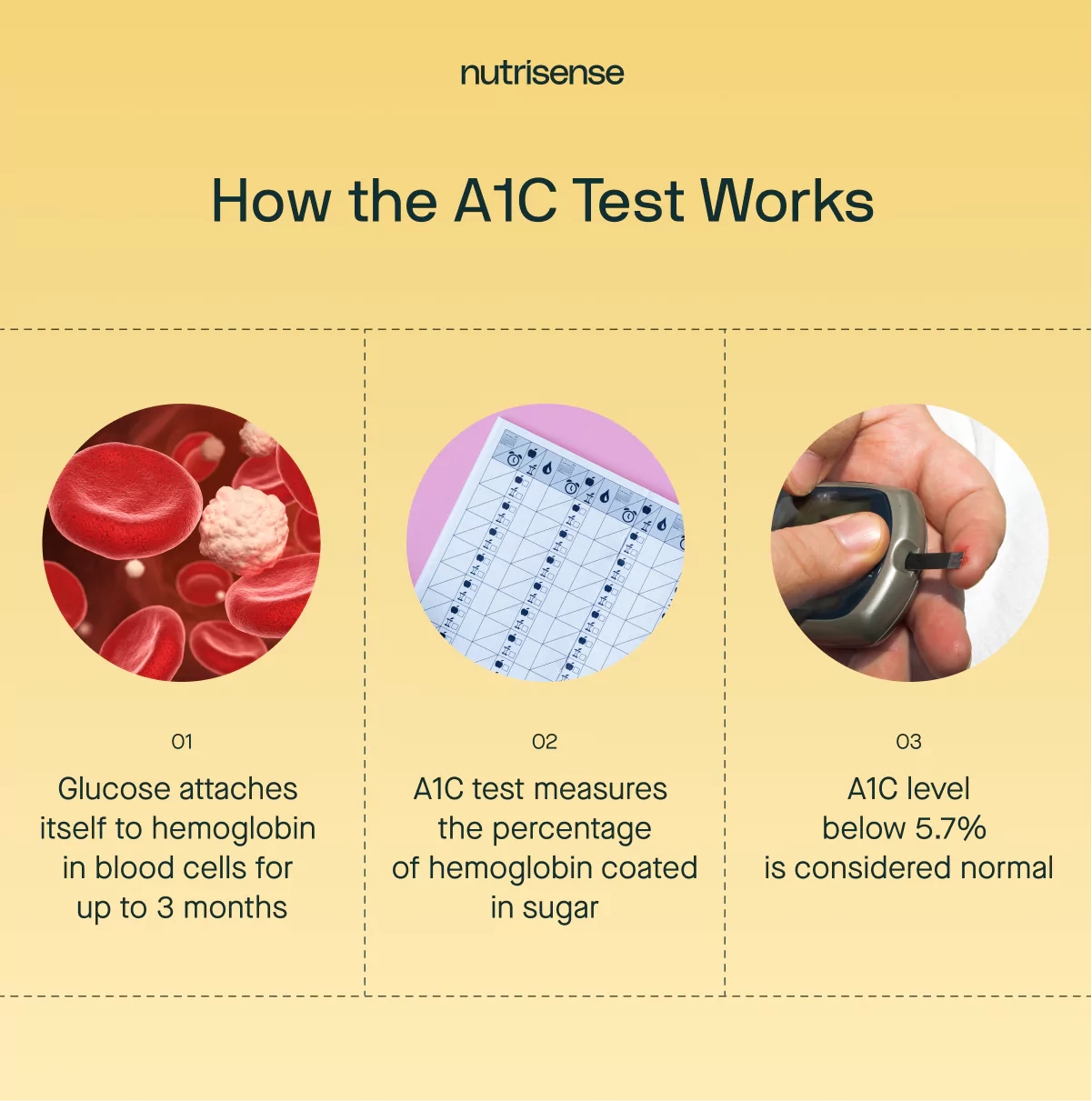
Also known as an HbA1c test, an A1C test measures your average glucose level over the past two to three months. Instead of measuring the amount of glucose in your bloodstream, your A1C level represents the percentage of hemoglobin in your red blood cells that is coated in glucose.
When glucose enters your bloodstream, it attaches itself to hemoglobin. Everyone has some glucose attached to hemoglobin in their blood cells, but people with high glucose levels have higher levels.
A1C ranges
An A1C test is a type of glucose test used to diagnose prediabetes and diabetes. An A1C less than 5.7 percent is considered normal. Generally, an A1C between 5.7 and 6.4 percent is considered prediabetes, and 6.5 percent or higher is considered diabetes.
To see an estimate of your A1C levels, try our A1C level calculator here.
Who should get an A1C test?
According to the Centers for Disease Control and Prevention (CDC), A1C testing is recommended for those who have already been diagnosed with diabetes, adults over 45, and those who are under 45 but are overweight or have one or more risk factors for prediabetes or type 2 diabetes.
If you have prediabetes, you should repeat an A1C test as often as your healthcare provider recommends.
Other tests used to identify prediabetes
A1C is one of several lab tests used to identify prediabetes. Fasting plasma glucose and the oral glucose tolerance test are also standard options your clinician may use.
- Fasting plasma glucose FPG: A single plasma draw after at least 8 hours with no caloric intake. Many guidelines flag 100 to 125 mg/dL as the range often labeled prediabetes.
- Oral glucose tolerance test OGTT: You drink a 75-gram glucose beverage, then plasma glucose is checked, most often at 2 hours. A two-hour value of 140-199 mg/dL is commonly used to indicate impaired glucose tolerance.
- Random plasma glucose RPG: Drawn without regard to the last meal. Often used when symptoms suggest diabetes, and it is not typically used to define prediabetes on its own.
These labs provide a point-in-time view, whereas A1C reflects about three months' worth of data.
Between lab visits, health tech like a glucose biosensor or continuous glucose monitor (you get the most benefit when you use it with a program like Nutrisense) displays 24/7 glucose patterns measured in interstitial fluid, allowing you to see how meals, activity, stress, and sleep impact your day-to-day levels.
Use CGM data in conjunction with your clinician’s guidance and standard laboratory tests.
What is prediabetes, and who is at risk?
Prediabetes is a condition in which glucose levels are higher than normal, but not high enough to be diagnosed as type 2 diabetes. Anyone can develop prediabetes, even if you’re not overweight, but certain people may be at higher risk. Risk factors for prediabetes include:
Risk factors
- Being 45 years or older
- Being obese or overweight
- Having a family history of diabetes
- Living a sedentary lifestyle or being physically active less than three times a week
- Having a history of gestational diabetes
- Being of a certain ethnicity, such as African American, Hispanic, American Indian, or Alaskan Native, Pacific Islander, or Asian American
That "borderline" A1C number
You leave your annual check-up with the lab report in your hand. You’ve been working hard, trying to make better choices, but the number is right there in black and white: an A1C of 5.8%.
Your doctor called it "prediabetes" and told you to watch your diet, but you thought you already were. The news feels frustrating and confusing, leaving you wondering what you’re missing and what real changes will actually move that number.
Prediabetes vs. diabetes
Diabetes is a chronic condition where the body either doesn't produce enough insulin or is unable to effectively use the insulin it produces. This leads to consistently elevated glucose levels, which can have serious long-term health consequences such as cardiovascular disease and kidney failure.
On the other hand, prediabetes is a condition where glucose levels are higher than normal but not yet high enough to be classified as a diagnosis of diabetes. It serves as a warning sign and an opportunity for early intervention.
People with prediabetes have a high risk of developing type 2 diabetes and other associated health complications. However, studies also show that prediabetes can be reversed with lifestyle changes like healthy eating, regular exercise, and weight management.
Signs of prediabetes
Prediabetes often has no signs or symptoms and can only be diagnosed by a doctor through glucose tests such as an oral glucose tolerance test or a fasting plasma glucose test.
However, there are possible warning signs that prediabetes has progressed to type 2 diabetes, and these include:
- Increased hunger or thirst
- Frequent urination
- Fatigue
- Blurred vision
- Numbness or tingling in the hands and feet
- Frequent infections or slow-healing sores
- Unintended weight loss
Treatment for prediabetes

Treatment for prediabetes primarily focuses on lifestyle changes that improve glucose control and lower the risk of diabetes. These can include weight loss if you’re overweight, healthy eating, regular physical activity, and stress management.
Some people with prediabetes or diabetes are treated with medications, including Biguanides, Thiazolidinediones, α-Glucosidase Inhibitors, and GLP-1 agonists. However, treatment and management of prediabetes is not a one-size-fits-all approach, and is usually personalized based on an individual's specific needs and medical history.
Collaborating with healthcare professionals, including dietitians and exercise specialists, can provide valuable guidance and support when developing a diabetes prevention program or plan.
Find the right Nutrisense programto turn insight into progress.
Know the “why” behind your A1C and change what shapes it with Nutrisense
Know the “why” behind your A1C and change what shapes it with Nutrisense
6 healthy ways to keep your A1C levels low
Keeping your A1C levels at a healthy level is important for your overall health. Luckily, there are plenty of steps you can take that can support optimal A1C levels, including dietary changes, physical activity, and healthy lifestyle changes.
Here are a few of the things you can do:
1) Build a nutrient-rich meal plan
A nutritious meal plan plays a crucial role in keeping A1C levels low and managing glucose effectively. Here are some tips for building a nutrient-rich meal plan:
- Incorporate a diverse range of nutritious foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats into your meals. Each of these provides essential nutrients that contribute to overall health.
- Focus on fiber-rich foods, such as non-starchy vegetables and legumes, as they help slow down digestion and may prevent rapid glucose spikes. However, carb-containing foods may not all be tolerated equally for those with prediabetes, and testing your personal tolerance is important.
- Include lean sources of protein, such as poultry, fish, tofu, legumes, and low-fat dairy, in each meal. Protein helps regulate glucose levels, supports muscle and tissue health, and helps to maintain a healthy weight.
- Opt for sources of healthy fats, such as avocados, nuts, seeds, olive oil, and fatty fish, which provide essential fatty acids and promote cardiovascular health.
2) Manage portion sizes and track carb intake

Being mindful of your portion sizes and carbohydrate intake can contribute to healthy A1C levels. The American Diabetes Association advises monitoring the amount of carbs you eat at each meal or snack to prevent sharp spikes or prolonged glucose elevations.
Carbohydrates are broken down into glucose during digestion and can cause glucose spikes when consumed in large amounts. Make sure to pair your carbs with a source of protein and fiber to reduce the chance of higher glucose spikes.
3) Commit to regular exercise
Getting the right amount of exercise plays a crucial role in keeping A1C levels low and managing your glucose. Physical activity enhances insulin sensitivity, allowing the body to use insulin more effectively.
Appropriate amounts of exercise also support weight loss and weight maintenance efforts, which is important for managing A1C levels. Excess weight and obesity are risk factors for the development or worsening of insulin resistance, which can negatively affect glucose control. However, overtraining or improper fueling for your workouts can backfire, adding more metabolic stress and potentially raising glucose levels. So finding the right balance is important.
4) Partner with a certified nutrition professional
Partnering with a qualified nutritionist can provide you with specialized guidance, education, and support to make healthy dietary decisions and effectively manage glucose levels. A nutrition professional, such as a registered dietitian or a certified nutrition specialist, can provide individualized guidance and dietary support tailored to your unique needs, preferences, and health goals.
They can also take your unique medical history, lifestyle, cultural background, and dietary restrictions into account. They can help you make practical meal plans that align with your dietary goals and glucose targets, which can be especially useful in managing your A1C levels.
5) Address stress and mental well-being

Addressing your mental health is important for your physical health. Emotional stress can trigger the release of stress hormones like cortisol and adrenaline, which can raise glucose levels.
Prolonged or chronic stress from a variety of sources can lead to sustained elevated glucose levels, making it difficult to maintain healthy A1C levels. Try managing your stress levels by properly fueling your body with the nutrients it needs to function, getting enough sleep, practicing breathing techniques, meditating, or engaging in other stress-relieving activities. You can also try 1:1 sessions with a stress management specialist (like the ones at Nutrisense), to learn how to shift your body out of fight-or-flight and restore your metabolism.
6) Track your glucose
Regular monitoring of glucose levels can increase your awareness and understanding of how different factors, like diet, physical activity, medication, stress, and sleep, affect your glucose levels. One innovative solution to tracking your glucose is using a glucose biosensor and a continuous glucose monitor (CGM).
This device continuously monitors glucose levels throughout the day, offering 24/7 insights into glucose trends and patterns. Through a program like the Nutrisense program, you’ll also receive personalized guidance from registered dietitians and nutritionists that can help you interpret your glucose data, provide recommendations, and support you in making meaningful changes to your lifestyle.
Turn A1C insights into action with Nutrisense
Knowing your A1C is just the starting point. Nutrisense helps you see what’s behind the number, and how small, daily choices impact your glucose 24/7. With personalized data and 1:1 dietitian support, you’ll learn to fine-tune your routine and build habits that last.
Dietitian guidance
Sign up to access insurance-covered video calls with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Program and app
With the Nutrisense Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitors (CGMs), and analyze the trends over time in the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Take our quiz
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.
A1C and prediabetes FAQ
Q1. How do A1C and CGM data differ, and how should I use them together?
A1. A1C is a lab test that reflects a multi-month average of your glucose. A tool like a glucose biosensor or CGM shows 24/7 trends of glucose measured in interstitial fluid, revealing how meals, movement, stress, and sleep affect you day to day. Many people use A1C for long-range tracking and biosensors or CGMs to guide daily adjustments.
Source: What is a CGM
Q2. Can Nutrisense estimate my A1C from CGM data?
A2. Yes. Our A1C calculator estimates A1C from average glucose. Use it to get a directional view between lab tests. It does not diagnose or replace lab testing. If your estimate and lab results differ, share both with your clinician and use CGM patterns to fine-tune meals, activity, and sleep.
Source: How to Calculate A1C Levels
Q3. My A1C is normal, but I see frequent glucose spikes on my CGM. What does that mean?
A3. A1C averages many days of data, so short peaks and dips can be masked. CGM highlights the timing and magnitude of swings so you can experiment with meal composition, order, timing, and post-meal activity. If patterns concern you, review them with your clinician and a Nutrisense dietitian for personalized next steps.
Source: Everything You Should Know About the Glucose Curve
Q4. Do I need a prescription for sensors, and how long does each one last?
A4. The glucose biosensors used with Nutrisense are over-the-counter and do not require a prescription. Members typically receive two sensors per month. Each sensor measures glucose in interstitial fluid and is worn for up to 15 days once activated. Shipping is available in the United States. You can use the Nutrisense program even if you have your own prescription CGM, with the bring-your-own-sensor options.
Source: How Nutrisense Works
Q5. How does Nutrisense support people with prediabetes between A1C checks?
A5. Nutrisense pairs 24/7 glucose trends from a biosensor with the option to sign up for 1:1 (insurance-covered) video call guidance from a registered dietitian. Together, you can test meals, movement, stress management, and sleep routines to see what works for you, then build sustainable habits. Nutrisense does not diagnose or treat conditions. Use glucose biosensor and CGM insights to complement your clinician's regular A1C testing.
Source: CGM Benefits for Prediabetes
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Liz has a Master of Science degree in Clinical Nutrition and Integrative Health and is a board-certified nutrition specialist (CNS) and a licensed dietitian nutritionist (LDN). As a nutritionist, Liz has educated and counseled 100s of clients in areas such as weight loss, hormonal imbalances, and gastrointestinal diseases.




