Glycogen vs Glucose: How They Work Together
.webp)
Key Takeaways
Whether you're trying to understand blood sugar levels, optimize your diet or improve overall fitness, knowing more about the relationship between glucose and glycogen is an important part of the puzzle.
Glucose and glycogen are similar yet slightly different carbohydrate molecules that your body relies on to regulate energy balance for many metabolic functions.
- Glucose is a single sugar unit or monosaccharide.
- Glycogen is a multi-sugar unit or polysaccharide.

Maintaining normal blood glucose levels is considered a top priority by the body. It does this through various mechanisms involving key hormones like insulin and glucagon. Wondering what some other areas of glucose and glycogen metabolism are? Read on as we take you through some important areas below.
Understanding Glycogen and Glucose
Your body can make glucose in certain situations, but most of what it uses comes from foods you eat.
For example, you consume various simple and complex carbs when you eat carbohydrate-containing food such as fruit, grains, or starchy vegetables.
Simple carbs include:
- Monosaccharides (One sugar unit)
- Disaccharides (Two sugar units)
Complex carbs include:
- Oligosaccharides (Three to 10 sugar units)
- Polysaccharides (> 10 sugar units)
Here's an interesting fact: Glucose is the most abundant monosaccharide found in nature! Other monosaccharides include fructose and galactose. Monosaccharides can come together to create disaccharides like sucrose (glucose + fructose) and lactose (glucose + galactose), among others.
{{rich-text-cta-cgm1="/style-guide"}}
As your digestive processes break down various carbohydrates, glucose is often the star end product. Your gastrointestinal tract absorbs glucose into the blood. Your cells then use it as a primary energy source, supplying fuel for thousands of life-sustaining functions. As we've discussed earlier, your blood sugar levels tell you about the amount of glucose or concentration in your blood.
Your liver and skeletal muscles often store excess glucose. It can also be converted into fatty acids, which travel to other parts of the body and are stored as fat in adipose tissue.
Glycogen is a polysaccharide containing many branched chains of glucose molecules, acting as the primary storage form of glucose in the body. The amount of glycogen stored in the body depends on many factors, including your physical fitness/training level, basal metabolic rate, eating habits, and disease state(s).
What is Glucose?
As we now know, glucose is the most abundant monosaccharide and the sugar we refer to when we talk about blood sugar. Remember, it’s normal for your blood glucose levels to fluctuate to some degree. Depending on your activity level, the time of day (or night), and the state of other dietary and lifestyle factors, glucose levels may vary.
Most cells in your body depend upon a continuous supply of glucose to create energy in the form of adenosine triphosphate—also known as ATP. When your body breaks this glucose down, it harvests energy in the form of high-powered chemical bonds found in the ATP molecule.
This energy, along with the help of enzymes, is then used to execute many reactions of metabolism. At rest, each muscle cell houses around a billion ATP molecules. These ATP molecules are fully used up (and replaced) every two minutes. During higher intensity exercise, ATP production can increase 1000-fold to meet the demand of the working muscle.
For your cells to use glucose, they rely on a transport system that allows the glucose to move in and out of them. There's also a family of protein carriers called glucose transporters (GLUT) is also involved in this process.
Elevated blood glucose levels trigger insulin release by the pancreas. Insulin binds to a specific receptor site on the muscle and fat cells, interacting with one of the GLUT family proteins to help “open the gate” for glucose to enter the cell.
What is Glycogen?

Glycogen is the body's primary storage form of carbohydrates, existing as a polysaccharide composed of many glucose molecules that are connected together.
In humans, the majority of glycogen (~500 grams) is in skeletal muscles and ~100 grams in the liver. However, since you have far more muscle mass than liver mass (by weight), proportionally, your liver ends up being the larger site of glycogen storage.
The balance by which glucose is removed from the blood into skeletal muscle glycogen is the major determinant of insulin sensitivity. In addition to muscle and liver cells, your brain cells, heart cells, smooth muscle cells, kidney cells, red and white blood cells, and even adipose cells store small amounts of glycogen.
So, What is Glycogenesis?
Glycogenesis is the process of turning glucose into glycogen. Liver glycogen is more important than skeletal muscle glycogen in maintaining blood glucose balance—especially during periods of fasting.
However, the glycogen stores found in muscle are essential for your fight or flight response. Insulin stimulates glycogen synthesis in the liver and skeletal muscle. Some sources suggest that 20 and 30 percent of the carbohydrate intake from a mixed macronutrient meal will end up stored in the form of glycogen in the liver and skeletal muscle, respectively.
Unfortunately, there are many reasons the process of glycogen creation can become impaired. And people with type 2 diabetes and insulin resistance have reduced glycogen in the liver and skeletal muscle.
Here's something else to consider: if you've heard that low-carb diets can cause the loss of “water weight," you've probably wondered why that is. Each gram of glycogen is stored with at least three grams of water. As you shift into a very low-carb dietary approach, some of your glycogen stores may become depleted. As you lose glycogen, you will also lose some water.
{{rich-text-cta-member-stories="/style-guide"}}
Exercise and Glycogen
When you exercise, your skeletal muscles take up glucose from your blood and break muscle glycogen stores down for fuel. During physical activity and depending on the intensity of the exercise, the muscle may increase glucose uptake seven to 20 times the basal level.
Physical training improves insulin sensitivity in the peripheral tissue and can improve impaired glucose tolerance. The rate at which your body breaks down muscle glycogen depends upon the intensity of physical activity. Typically, the higher the exercise intensity, the greater the rate at which muscle glycogen is degraded.
What does all of this mean? Simply put, high-intensity activity can quickly lower glycogen stores in active muscle cells, even if the total workout time is short.
On the other hand, an endurance athlete who trains for many hours at a time will also experience a marked decline in muscle glycogen, but this may happen at a much slower rate.
What are Glucagon and Insulin?
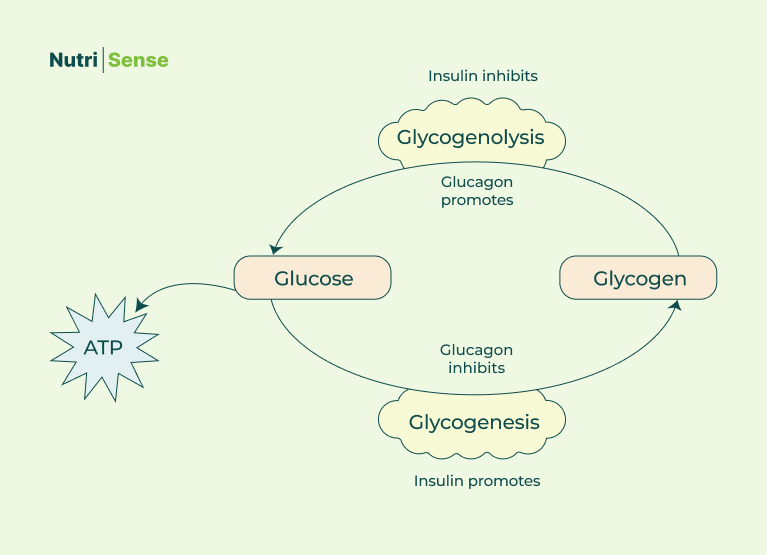
Specific hormones regulate the process of creating glycogen from glucose and liberating glucose from glycogen stores.
As we’ve discussed elsewhere, glucagon and insulin are two of the main hormones regulating this energy balance in the body. Glucagon and insulin have opposite yet complementary functions. The pancreas makes both hormones:
- Pancreatic alpha cells produce glucagon
- Pancreatic beta cells produce insulin
Insulin stimulates the creation of more glycogen (glycogenesis) and inhibits the breakdown of glycogen (glycogenolysis). Glucagon does the opposite—it inhibits glycogen generation (glycogenesis) and promotes its breakdown (glycogenolysis).
In a nutshell, when your glucose falls too low, your body secretes glucagon to help raise your glucose levels. When your glucose levels rise, your body secretes insulin to help lower them.
Beyond Glucagon and Insulin

Though glucagon and insulin are the most famous hormones in glucose and energy homeostasis, other important players exist. These include amylin, GLP-1, glucose-dependent insulinotropic peptide (GIP), epinephrine, cortisol, and growth hormone.
Stay tuned for our next article in this series to learn about these and for more information on glucose homeostasis!
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Jordyn has a bachelor’s degree in biology, a graduate degree in Human Nutrition and completed a dietetic internship at the Memphis VA. She's a dietitian at Nutrisense, and has experience working as a clinical dietitian at a VA medical center specializing in oncology and at the Mayo Clinic, working with a wide range of patients ranging from neonates in the NICU to adult ICU.




