5 Key Metabolic Markers: What They Mean for Your Health

Key Takeaways
What are metabolic markers?
Metabolic health is a hot topic in today’s healthcare arena, and for good reason - very few Americans are considered metabolically healthy, even among people who are not overweight.
Metabolic health doesn’t always have a clear definition, but it is generally accepted as including normal levels of five measurable characteristics known as metabolic markers.
When Your Lab Results Raise More Questions
You just got the results from your annual physical. You scan the page, seeing numbers next to terms like "triglycerides" and "fasting glucose." Your doctor mentioned they were a bit high, but the report doesn't explain how these markers connect to your daily fatigue or the stubborn weight you've been fighting.
The numbers feel like a grade for a test you didn't know you were taking, leaving you to wonder if understanding them is the missing piece to making progress that finally sticks.
The five markers
Metabolic markers are used by health professionals to gauge someone’s overall health. These markers include blood pressure, glucose, triglycerides, high-density lipoprotein and low-density lipoprotein cholesterol, and waist measurement.
So what makes these specific metrics so important for overall health? Read on to learn all about metabolic health markers and how to keep them in check.
What is metabolic syndrome?

When metabolic health is compromised, it can lead to a wide range of health concerns and conditions. One of these conditions is known as metabolic syndrome. Metabolic syndrome refers to a cluster of physical conditions that can lead to an increased risk of heart disease, stroke, diabetes, and other chronic diseases.
Diagnostic criteria
Metabolic health markers are often used to determine if a patient has metabolic syndrome. You may have metabolic syndrome if you have three or more of the following:
- High fasting glucose
- High cholesterol
- High triglycerides
- High blood pressure
- High waist circumference
Let’s take a look at each of the individual markers of metabolic health and how to know whether or not they’re in the normal range.
1) Glucose levels
Glucose is one of the most important metabolic markers. Having glucose levels that are chronically higher or lower than normal or having a high glycemic variability can put you at a greater risk of metabolic disease and a number of chronic health conditions.
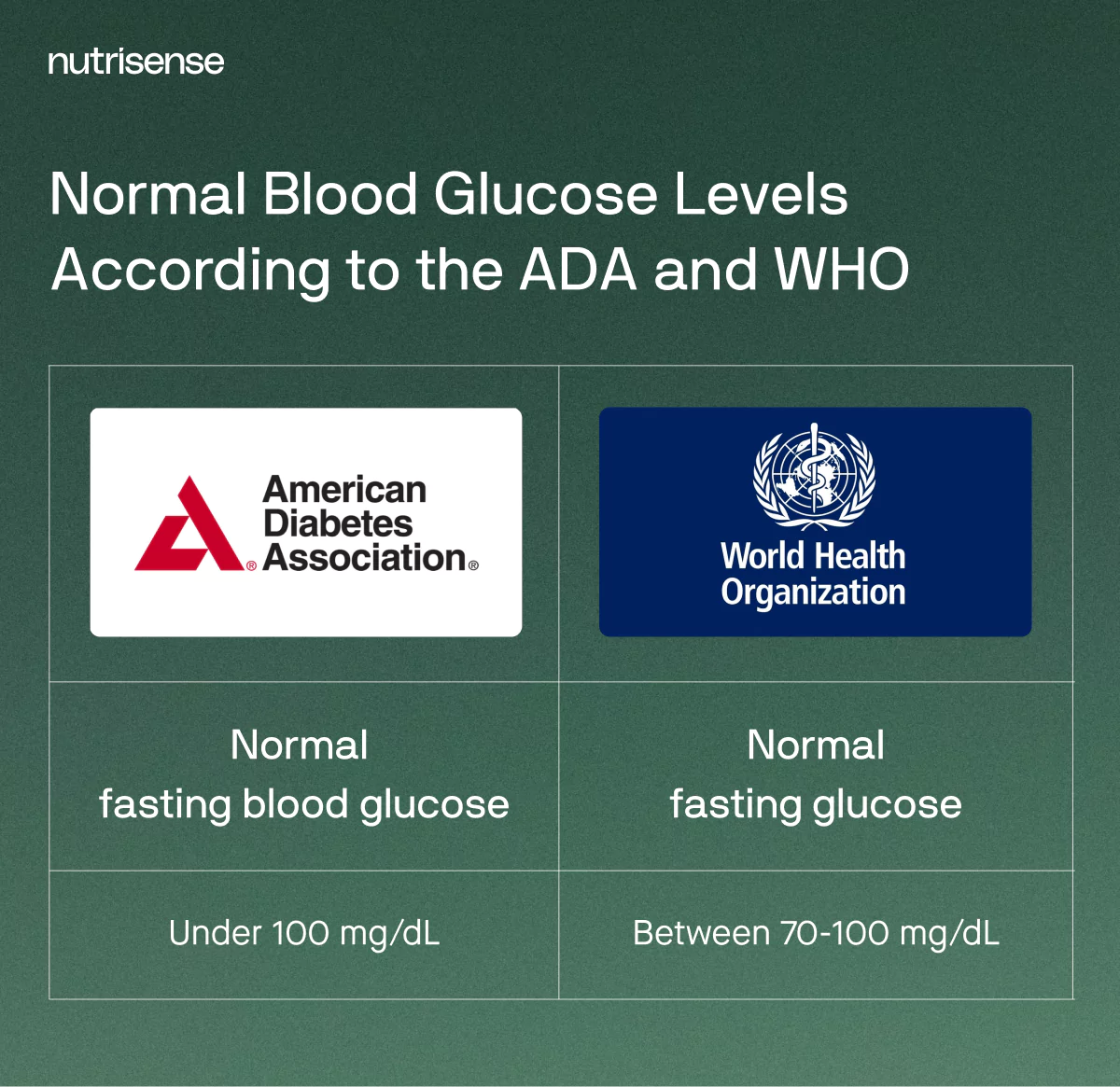
Fasting targets
Fasting glucose is measured during a fasting state - meaning you haven’t had anything to eat or drink for at least eight hours. A normal fasting glucose is generally considered to be less than 100 mg/dL, according to the ADA, while higher levels could be a sign of prediabetes or diabetes.
High glucose risks
Glucose that is too high is called hyperglycemia, and over time, chronically high levels can lead to type 2 diabetes mellitus, heart disease, stroke, nerve damage, fatty liver disease, kidney damage, and vision loss. Over time, it can also cause insulin resistance, which may cause changes in how your pancreas produces insulin and how your cells respond to insulin.
Low glucose symptoms
Low glucose is called hypoglycemia. Having frequent episodes of hypoglycemia can cause symptoms like brain fog, fatigue, lightheadedness, anxiety, and heart palpitations.
HbA1c and fasting insulin: extra markers that round out the picture
Beyond a single fasting value, two labs often used in clinics are HbA1c and fasting insulin. HbA1c estimates average glucose exposure over roughly 2 to 3 months and is used for clinical classification and target setting. See the American Diabetes Association’s Standards of Care on classification and targets for details: Classification and Diagnosis of Diabetes and Glycemic Targets.
If you use a continuous glucose monitor, remember it shows glucose measured in interstitial fluid with 24/7 trends. Pairing those day-to-day patterns with periodic HbA1c from your clinician helps you see both short and long horizons. Learn how sensors work in the Nutrisense app here: How it works.
- HbA1c is reported in percent and in mmol/mol. Your clinician can explain how it fits with your other labs.
- Fasting insulin is a single lab drawn after an overnight fast. Ask your clinician if it is appropriate for your check-ins.
- If tracking starts to feel rigid or all-consuming, focus on patterns rather than perfection, and consider meeting with a registered dietitian via Insurance-covered video calls.
2) Cholesterol levels
Cholesterol by itself is present in all the cells in your body, and is a type of fat that is essential for normal bodily functioning. Cholesterol includes substances in your body, such as:
- High-density lipoprotein (HDL)
- Low-density lipoprotein (LDL)
- Triglycerides
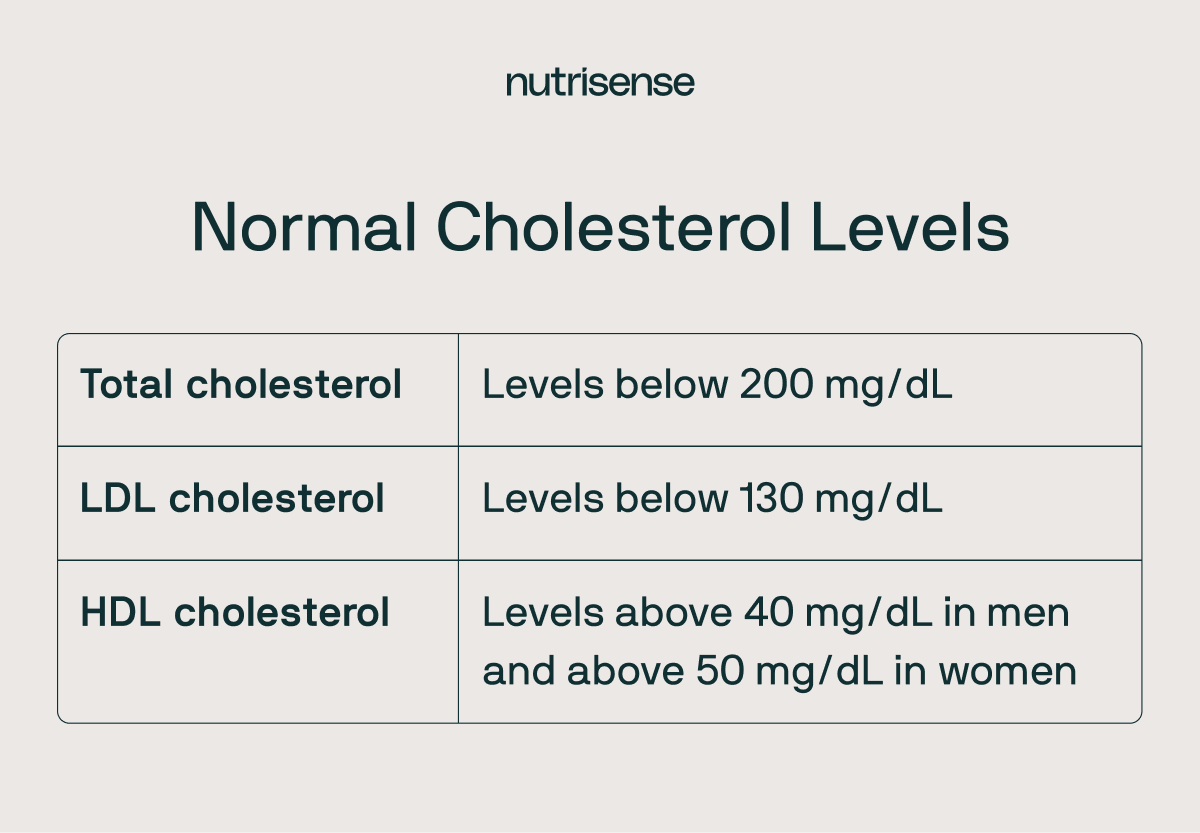
Optimal cholesterol ranges
It’s worth noting that there is some ongoing debate as to what optimal cholesterol levels may be. Additionally, recent research has even suggested that very high HDL-C levels are associated with an increased risk of all-cause death and cardiovascular death among men but not in women in the general population free of coronary artery disease. More research is needed to better understand these associations.
Cholesterol in and of itself is not considered good or bad. It is needed to help digest food, and to make hormones and some vitamins. Your body makes all the cholesterol it needs, but some dietary factors, like saturated fat, have been shown to increase cholesterol levels. However, the link between saturated fat and heart disease is not so straightforward.
HDL and LDL
Your liver makes most of the HDL and LDL that you need. In the body, HDL absorbs the cholesterol in your blood and takes it back to your liver. LDL cholesterol is also needed to carry cholesterol to our muscles, adrenal glands, gonads, and adipose tissues.
Lifestyle factors
However, levels of HDL cholesterol that are too low and levels of LDL cholesterol that are too high can be considered cardiovascular risk factors and may lead to a higher risk of having a heart attack or stroke. Factors like a lack of exercise, high stress, and excessive smoking can lead to high cholesterol levels.
3) Triglycerides
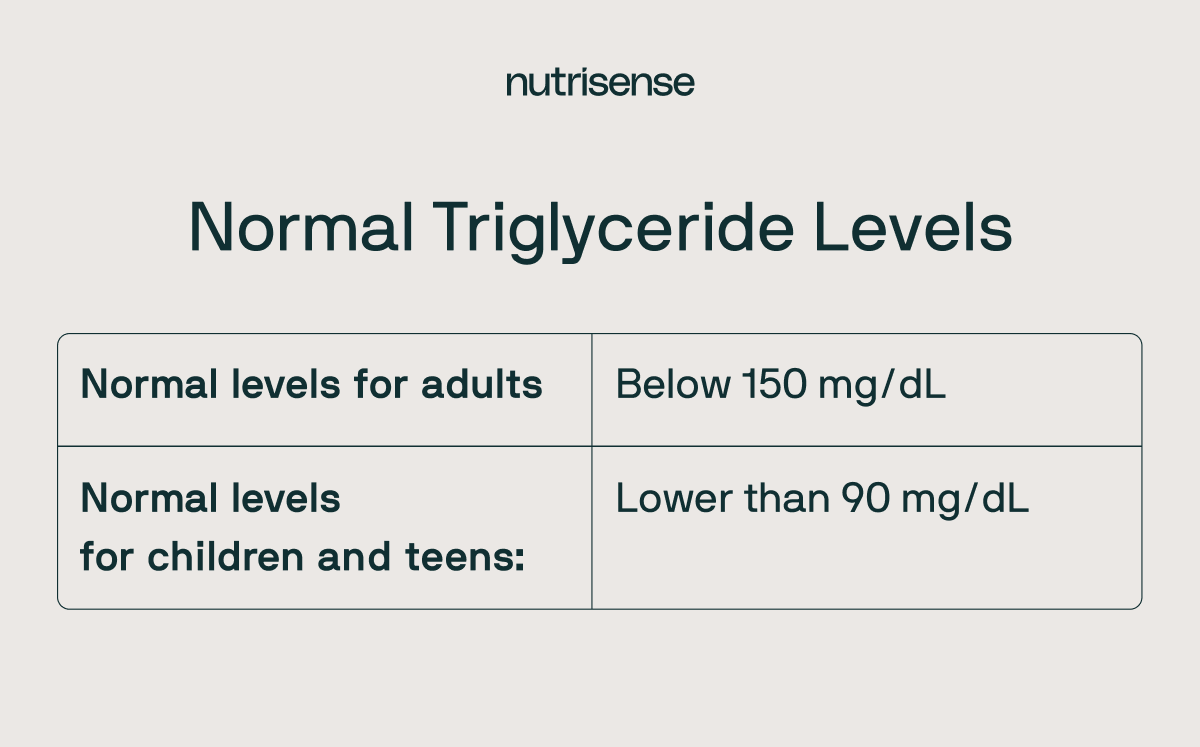
Having elevated triglycerides is another factor linked to cardiovascular disease. Triglycerides may become elevated as a result of dietary factors such as high intake of sugar and fat. There are some chronic conditions that can also cause higher than normal triglycerides, such as kidney disease, liver disease, diabetes, thyroid disease, and obesity.
Healthy range
A normal triglyceride level for adults is considered to be less than 150 mg/dL. Having higher than normal triglycerides can increase the risk of heart disease and metabolic syndrome.
4) Blood pressure
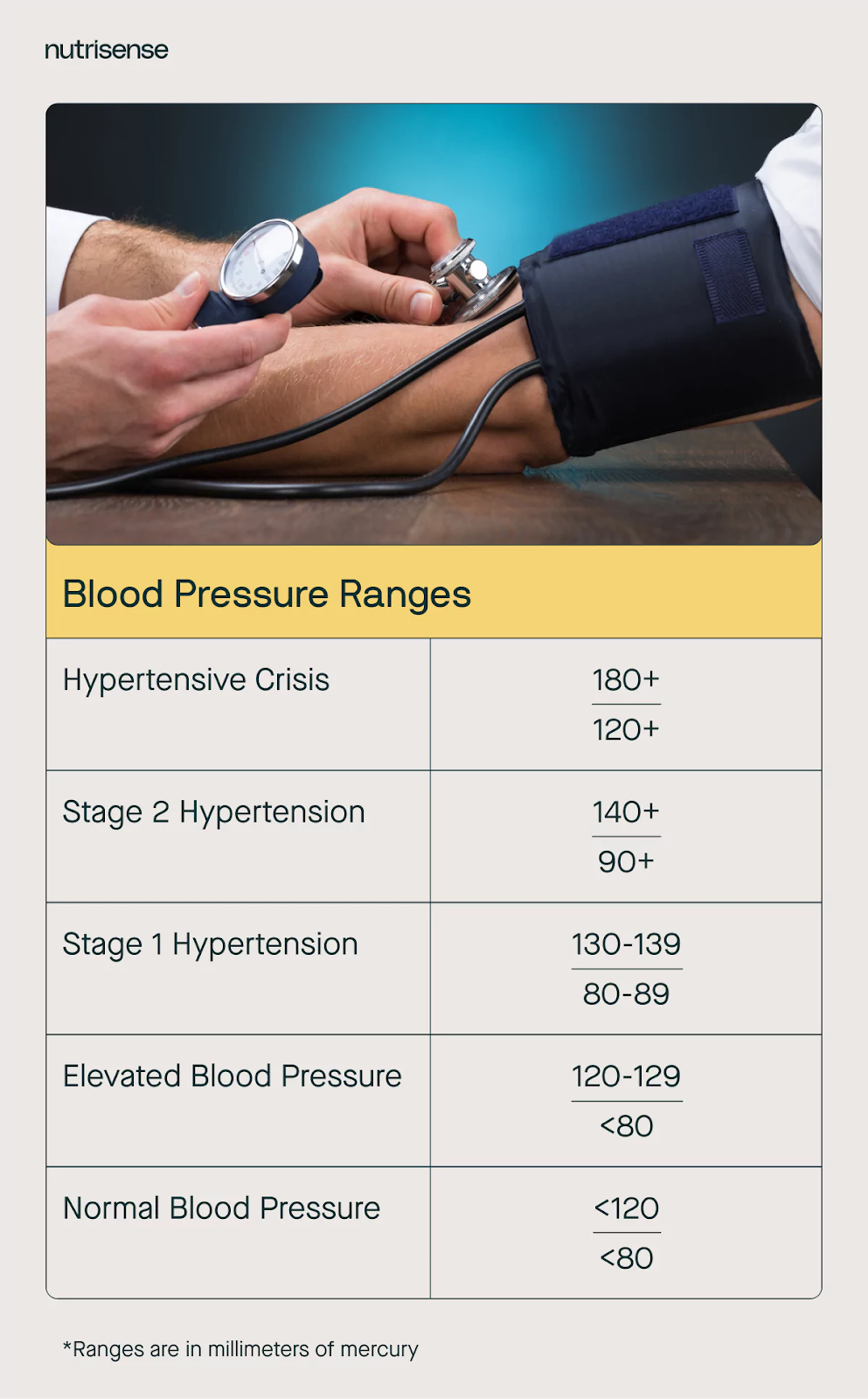
Your blood pressure is a measurement of the force your arteries use to pump blood throughout your body. Your systolic number (top number) represents the force on the artery walls when your heart beats and pumps the blood into your arteries. The diastolic number (bottom number) represents the pressure in your arteries when your heart is at rest between heartbeats.
If your blood pressure is consistently higher than 120/80, you’re at risk of developing stiff arteries, leading to high blood pressure, or hypertension. Arteries can become stiff due to several reasons, including:
- Genetics
- Dietary factors
- Physical activity
- High stress levels
Risks of hypertension
There are often no symptoms of high blood pressure, so it’s important to monitor your blood pressure regularly. High blood pressure can increase your risk of developing heart disease, having a stroke, developing hardening of your arteries, which leads to decreased blood flow, and even dementia.
Low pressure symptoms
On the other hand, low blood pressure or hypotension does have symptoms and can indicate other health issues such as neuroendocrine conditions, heart problems, and even low glucose. Symptoms of hypotension can include dizziness, lightheadedness, fainting, nausea, and trouble concentrating.
5) Waist circumference
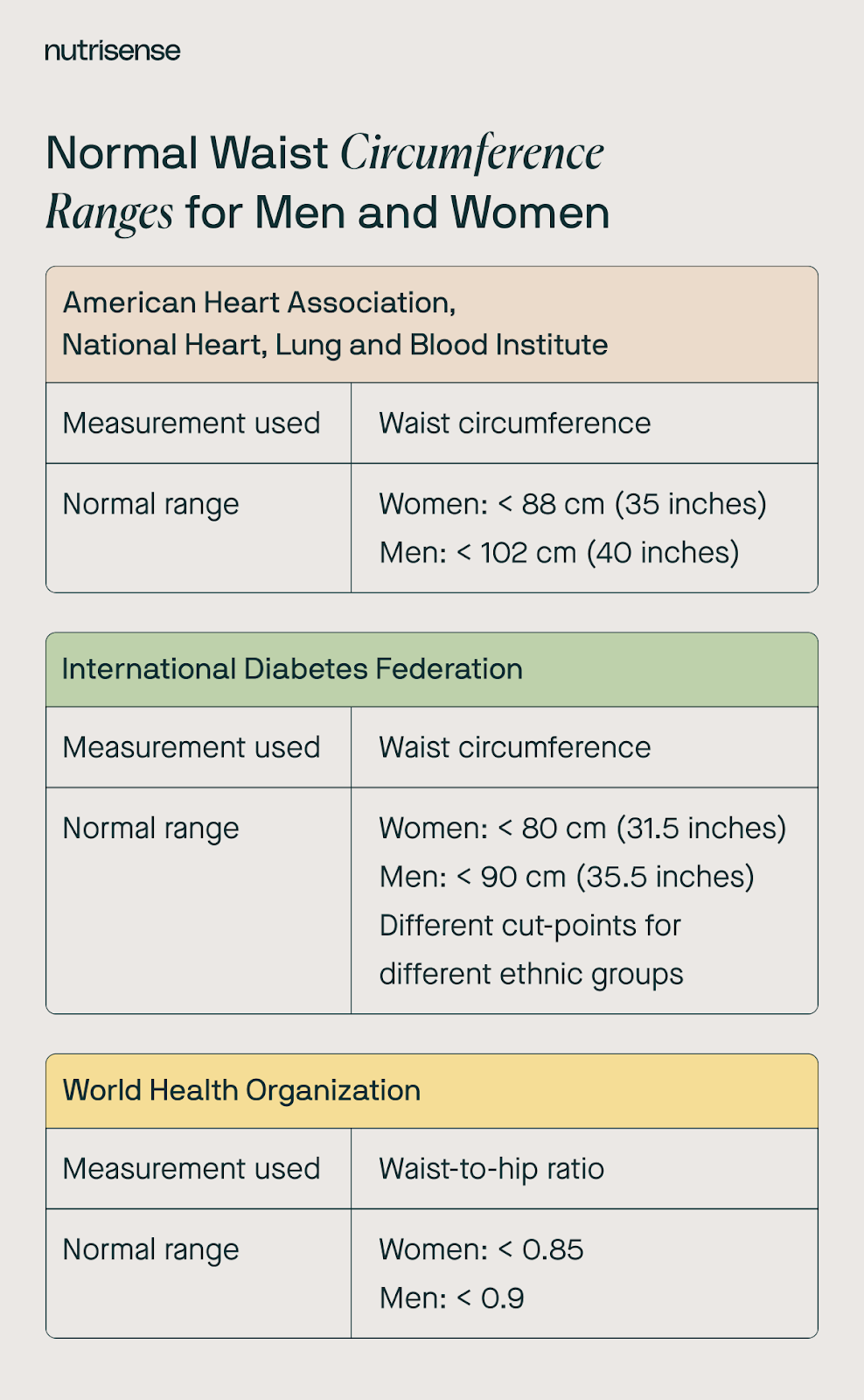
The last marker of metabolic health is your waist circumference. Your waist circumference is the measurement taken around your abdomen at the level of your belly button. Similar to the idea of a body mass index (BMI) test, this measurement can let you know if you may be generally at risk, though a more individualized assessment may be needed to confirm.
Visceral fat risks
Having excess fat around your abdominal area may be more dangerous to your health than having fat in other areas. This is because this “visceral fat” is metabolically active and increases your risk of heart disease, high blood pressure, diabetes, high cholesterol, and sleep apnea.
Thresholds
A normal waist circumference is 35 inches for non-pregnant women and 40 inches for men. If your waist circumference is higher than this, you’re at risk.
How can you manage and monitor these markers?

Your metabolic biomarkers have significant implications for your metabolic health, and these metabolic markers are connected, meaning that if one of your markers is abnormal, this may be a predictor of having other markers that are abnormal.
Luckily, it is possible to improve your markers and decrease your risk of metabolic syndrome and other health conditions with certain lifestyle changes and guidance from healthcare professionals and qualified nutritionists.
Choose Reliable Testing Methods
It’s important to choose reliable testing tools when you’re evaluating your metabolic markers. One common method to assess metabolic health involves blood tests that measure various biomarkers, such as glucose levels, lipid profiles, and insulin sensitivity.
Another way to stay on top of your metabolic health is through a continuous glucose monitor. A CGM allows you to see how your glucose levels fluctuate 24/7. This can provide valuable insight regarding what you eat, how exercise impacts your glucose, and even how your glucose changes while you sleep.
Eat a Balanced Diet

Eating a healthy diet is one factor that can help maintain healthy glucose levels and support weight loss or weight management for better metabolic health. While dietary needs can vary greatly from person to person, working to limit the amount of ultra-processed foods and high glycemic carbohydrates like sugar and refined carbs in your diet is a great way to get started. Focus on incorporating whole foods like fiber-rich fruits, vegetables, healthy fats, and lean proteins in your diet.
Get Appropriate Levels of Exercise
Increasing your physical activity can also make a big difference for your metabolic health. Adequate exercise can improve many metabolic markers, helping you to maintain a healthy, normal weight, regulate your glucose levels, and more.
Aiming for at least 30 minutes of moderate-intensity exercise most days of the week may be a good goal for many, though individual tolerance and needs should always be assessed when building the ideal exercise program.
Practice Good Sleep Hygiene
Practicing good sleep hygiene can also help optimize your blood pressure, glucose levels, and other metabolic markers. To obtain these benefits, avoid using devices that emit blue light at least an hour before bed, try to go to bed at the same time each night, and avoid drinking caffeinated or alcoholic beverages before bed or more generally if you are especially sensitive to these.
Your diet may also impact your sleep in a number of ways worth considering.
Manage Stress

Chronic stress can negatively affect all areas of your metabolic health. This type of stress can result in significant negative health effects that impact every aspect of health and function, including glucose regulation, lipid levels, blood pressure, and even weight.
Chronic stress can come in many forms, including ongoing nutrient imbalances, improper fueling for workouts, high levels of psychosocial pressure, and lack of sleep. Practicing stress-reduction techniques like yoga, meditation, or deep breathing exercises can help manage certain types of stress more effectively.
Find the right Nutrisense programto turn insight into progress.
FAQs about monitoring metabolic markers with Nutrisense
Q1. How does the Nutrisense biosensor measure glucose and how often is data captured?
A1. The Nutrisense biosensor measures glucose in interstitial fluid and records data about every 15 minutes. You scan with the Nutrisense app to sync readings and view 24/7 patterns across your day and night. This gives a continuous picture of trends instead of single snapshots.
Source: How it works
Q2. Do I need a prescription, and how long does each sensor last?
A2. No prescription is required for the over-the-counter sensors Nutrisense uses. Most memberships include two sensors per month, and each Stelo sensor lasts 15 days once activated. If you need a break, you can pause shipments in 30-day increments within your plan limits and apply sensors on your schedule.
Source: CGM Plans
Q3. Can I use Nutrisense if I do not have diabetes?
A3. Yes. Many members without a diabetes diagnosis use Nutrisense to learn how meals, exercise, sleep, and stress relate to glucose trends and to build practical habits with coaching. The program focuses on wellness and behavior change, not medical diagnosis or treatment. The app and sensors provide 24/7 trend data to guide small adjustments.
Source: CGM without Diabetes
Q4. What can I track in the Nutrisense app besides glucose?
A4. In the Nutrisense app, you can scan sensor readings and log meals, ingredients, exercise, sleep, and notes. You can view analytics like glycemic variability, set fasting windows, and track ketones if you measure them. These features help you run simple experiments and connect daily choices with your glucose data.
Source: Nutrisense App
Q5. What happens during a dietitian video call, and is insurance accepted?
A5. During video calls, a registered dietitian reviews your glucose patterns and logs, discusses goals, and lays out clear next steps. Many insurance plans cover these sessions, often with 0 dollars out of pocket. You can check eligibility in minutes and schedule at times that fit your routine, or self-pay if preferred.
Source: Nutritionist video calls
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough.
With Nutrisense, you can gain access to glucose biosensors, an intuitive mobile app for tracking your data, and expert guidance from nutritionists to help you better understand your metabolic health and customize your diet and lifestyle approach.
Dietitian support
Sign up to access insurance-covered video calls with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
App and sensors
With the Nutrisense Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitors (CGMs), and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Ready to take the first step?
Start with our quiz to find the right Nutrisense program to help you take control.

Heather is a Registered and Licensed Dietitian Nutritionist (RDN, LDN), subject matter expert, and technical writer, with a master's degree in nutrition science from Bastyr University. She has a specialty in neuroendocrinology and has been working in the field of nutrition—including nutrition research, education, medical writing, and clinical integrative and functional nutrition—for over 15 years.




