What is Metabolic Syndrome?

Key Takeaways
Metabolic syndrome is a group of five conditions that increase your risk for heart disease, stroke, and type 2 diabetes. A diagnosis is made when three or more are present: high glucose, low HDL cholesterol, high triglycerides, excess abdominal fat, or high blood pressure.
At a glance:
- Insulin resistance, where cells don't respond well to insulin, is considered a primary driver behind metabolic syndrome.
- Learn about the common clinical tests used for diagnosis, including a lipid panel and a fasting glucose test.
- The Nutrisense program is currently available only within the United States.
What is Metabolic Syndrome?
Sedentary time and convenience foods have increased the prevalence of metabolic syndrome.
Metabolic syndrome is defined as a cluster of interconnected risk factors that increase the likelihood of developing heart disease, stroke, and type 2 diabetes. The main risk factors of metabolic syndrome include:
- High blood pressure
- High glucose
- Excess abdominal fat
- Low HDL levels
- High levels of triglycerides
Diagnosis Threshold
A diagnosis of metabolic syndrome occurs when you have three or more of these health conditions. Understanding what metabolic syndrome is and how to avoid it can be paramount to your overall health.
In this article, we’ll cover the causes of metabolic syndrome, signs and symptoms to look out for, and lifestyle changes that can potentially help you lower your risk of developing this condition and improve your metabolic health.
What Causes Metabolic Syndrome?
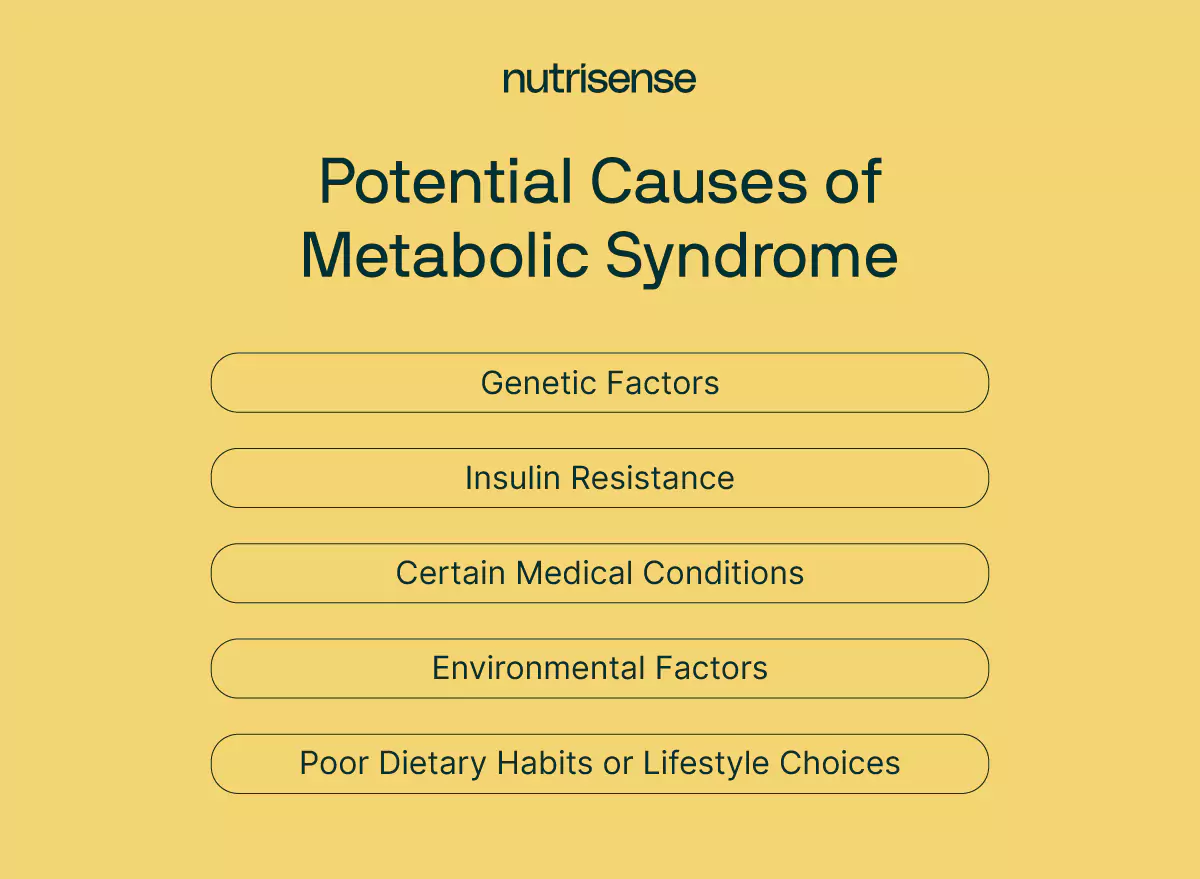
Many factors contribute to metabolic syndrome, and while some of these factors can potentially be avoided through lifestyle changes, others may be harder to avoid. Here are the causes of metabolic syndrome to be aware of.
Genetics
Certain people with a family history of this condition may be genetically predisposed to be more likely to develop metabolic syndrome. A study found that having family members with metabolic syndrome can increase your risk of developing metabolic syndrome. While you cannot change your genetics, you can take proactive steps to lower risk factors if you know this health condition runs in your family.
Insulin Resistance
Insulin resistance is the hallmark feature of metabolic syndrome. Insulin resistance occurs when your cells cannot correctly respond to insulin, leaving them unable to use the glucose in your blood for energy. Insulin resistance can lead to type 2 diabetes, cardiovascular disease, stroke, and other medical problems.
Several factors can increase your risk of developing insulin resistance, including:
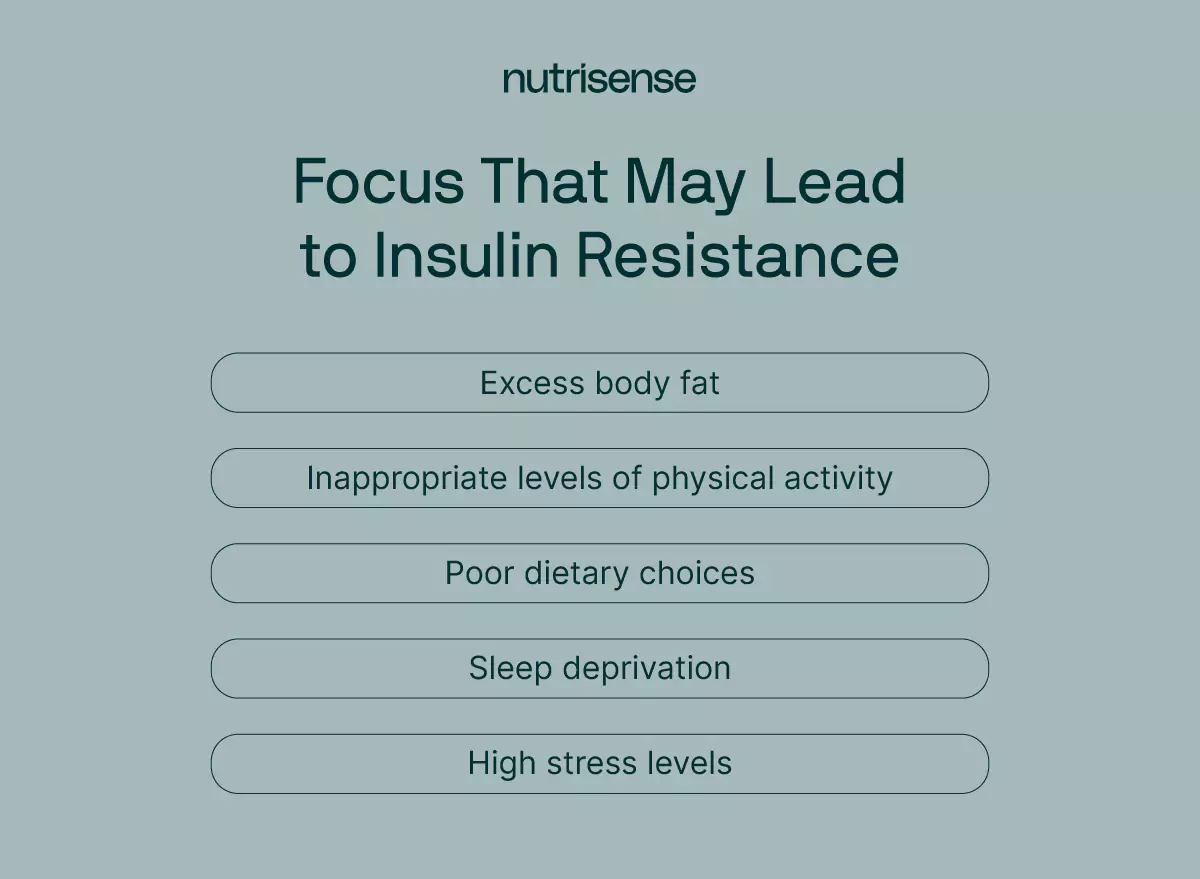
- Excess body fat
- Inappropriate levels of physical activity
- Poor dietary choices, such as excessive consumption of ultra-processed foods
- Sleep deprivation and high stress levels
Visceral vs Subcutaneous Fat
According to Dr. Brandy Zachary of the Functional Medicine Academy,
“Visceral fat stored in the abdominal cavity has a particularly adverse impact on metabolic health compared to subcutaneous fat. Visceral fat is metabolically active and produces higher levels of proteins and hormones that can drive insulin resistance, inflammation, and other metabolic abnormalities. Additionally, a sedentary lifestyle with low levels of physical activity leads to reduced glucose uptake in muscles and organs, worsening insulin resistance across bodily tissues.”
Other Medical Conditions
Medical conditions such as polycystic ovary syndrome, Cushing’s syndrome, hypothyroidism, and nonalcoholic fatty liver disease are also linked to an increased risk of metabolic syndrome.
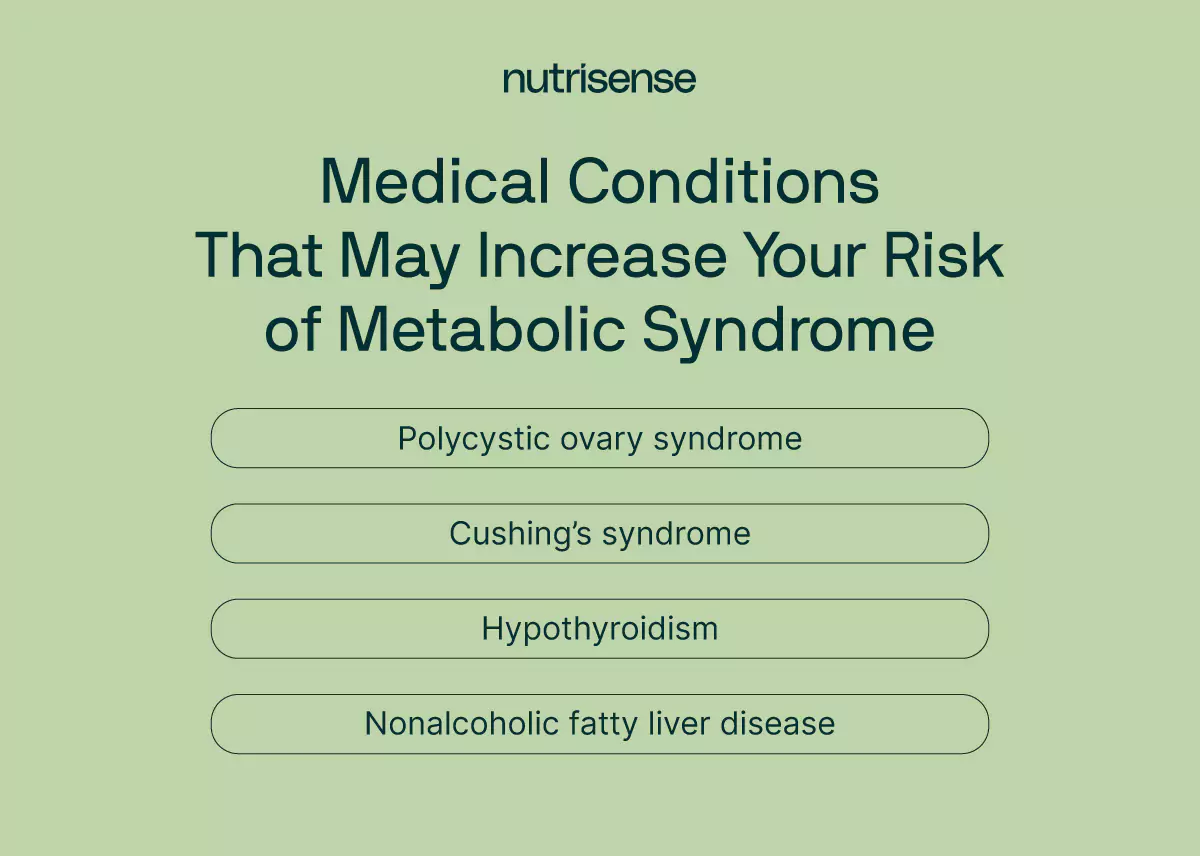
- PCOS: A hormonal disorder that can contribute to insulin resistance and other metabolic abnormalities.
- Cushing’s syndrome: A condition that results from excessive cortisol production, leading to weight gain and metabolic changes.
- Hypothyroidism: A condition linked to thyroid functioning that can lead to weight gain, high cholesterol, and other metabolic issues, including insulin resistance.
- Nonalcoholic fatty liver disease (NAFLD): A condition that can cause insulin resistance and metabolic syndrome, often a result of obesity.
Environmental Factors
Environmental factors such as air pollution can also be a factor leading to certain metabolic risk factors. According to research, excessive exposure to endocrine disruptor compounds like BPA and PFAs can lead to impaired immune function and increase your risk of conditions like type 2 diabetes and obesity.
Diet and Lifestyle
Implementing habits such as following a balanced and healthy diet, getting appropriate levels of physical activity, reducing stress, limiting alcohol, and not smoking can help you lower the risk of metabolic syndrome.
When your diet is unbalanced and you’re not physically active, you may be at a higher risk of obesity, high cholesterol, high triglycerides, high blood pressure, and diabetes—all the components of metabolic syndrome.
What are the Signs and Symptoms of Metabolic Syndrome?
There are many common signs and symptoms of metabolic syndrome. It is important to remember that just because you have one of the symptoms listed, it does not mean that you have metabolic syndrome. Three or more of these metabolic risk factors are required for a diagnosis of metabolic syndrome.
When 'Doing Everything Right' Isn't Enough
You leave the doctor's office with more questions than answers. Your blood pressure is still high, and your lab work shows elevated triglycerides. You’ve been consistently active and mindful of your diet, but your waist measurement is now over 35 inches.
It’s frustrating to feel like, despite all your effort, your body is working against you. As one member shares: “I feel more confident and I think I'm healthier and I understand how glucose work in my body.”
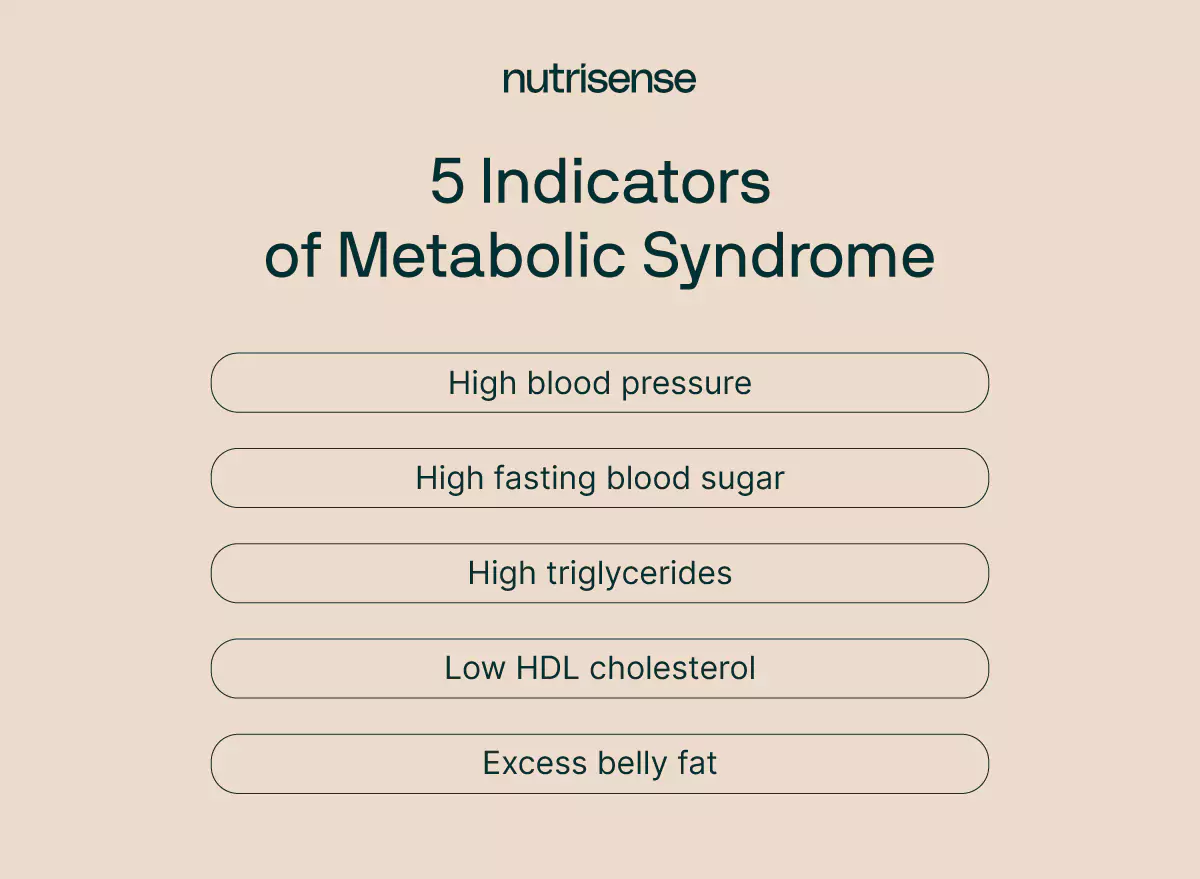
High Blood Pressure
High blood pressure is one of the common signs of metabolic syndrome. A normal blood pressure is 120/80 mmHg. Elevated blood pressure occurs when your systolic (top number) or diastolic (bottom number) pressure is higher than normal.
High Glucose
If your fasting glucose is consistently higher than 100 mg/dL, it is considered abnormal. A fasting glucose of 100-125 mg/dL is an indication of prediabetes.
High Triglycerides
Triglycerides are a type of fat (called lipids) that are found in your blood. When you eat more than your body needs, the excess calories are converted into triglycerides. A normal triglyceride level for adults is less than 150 mg/dL. High triglycerides can put you at risk for a heart attack, diabetes, stroke, and metabolic syndrome.
Low HDL Cholesterol

HDL cholesterol refers to the “high-density lipoprotein” in your blood. HDL cholesterol is called the “good” cholesterol because it helps remove other types of cholesterol in your blood. Having an HDL level lower than 40 mg/dL in men and lower than 50 mg/dL in women can indicate that you are at risk for metabolic syndrome and heart disease.
Excess Belly Fat
According to the American Heart Association, having a waist circumference above 35 inches (88.9 cm) for women and 40 inches (101.6 cm) for men is considered abnormal. Excess fat around the waistline that is associated with metabolic syndrome is sometimes described as “apple-shaped.”
If you experience abdominal obesity, your doctor may advise weight loss in order to reach a healthier body mass index (BMI).
Other Symptoms
Beyond the markers we’ve already discussed, other symptoms of metabolic syndrome may include:
- Increased thirst and urination
- Blurred vision
- Skin darkening on the back of the neck and skin folds
- Fatigue and weakness
How is Metabolic Syndrome Diagnosed?
If you possess any of the risk factors for metabolic syndrome, there are tests that your healthcare provider can conduct to determine if you have this condition or if you’re at risk.
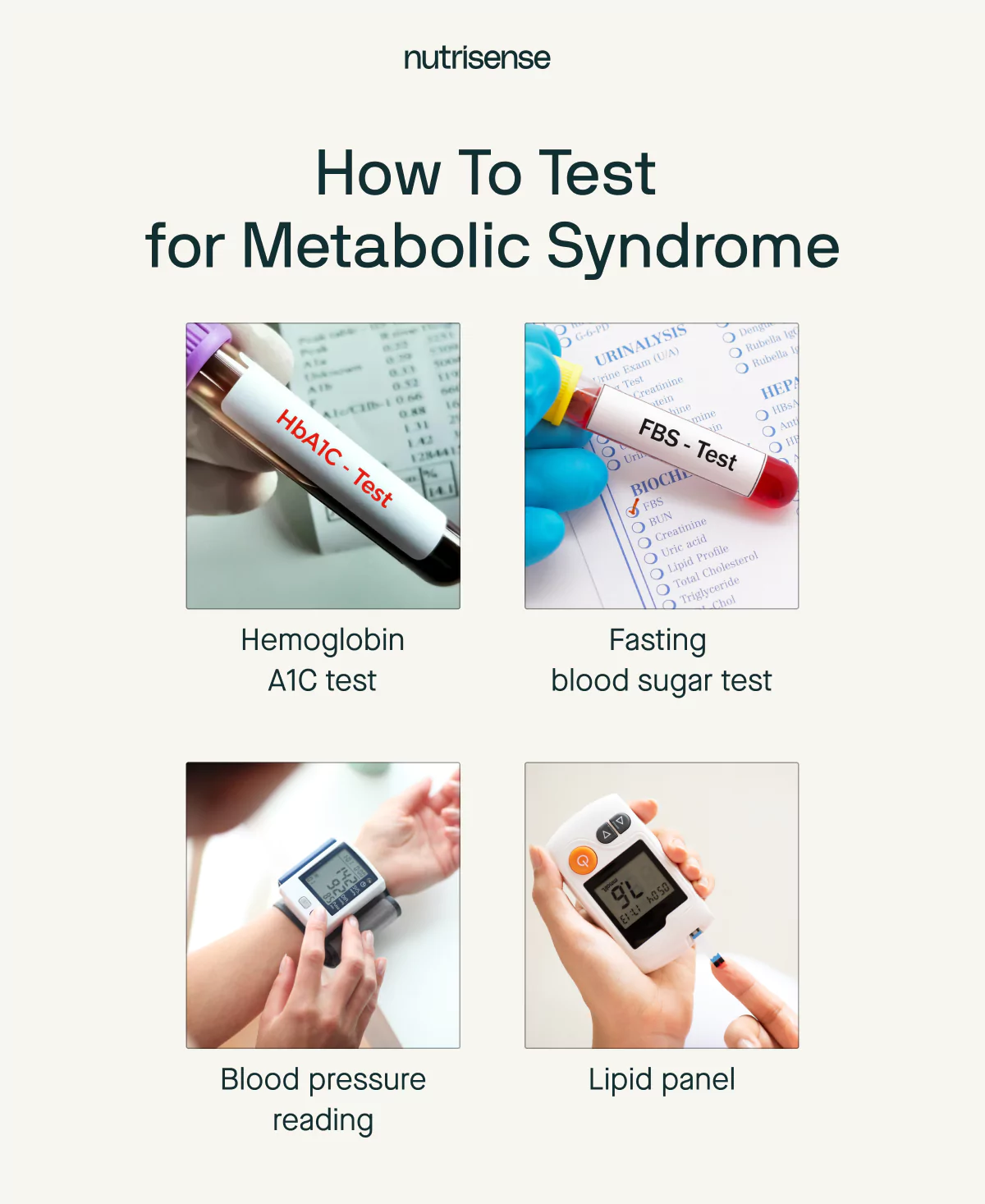
Fasting Glucose
A fasting glucose test is given after you’ve had nothing to eat or drink for the previous eight hours. Your healthcare provider will take a small amount of blood to measure the level of glucose present.
Blood Pressure Measurement
This test measures the force of blood flowing through your arteries using a blood pressure cuff placed around your upper arm or wrist. High blood pressure is a key component of metabolic syndrome.
Lipid Panel
This blood test measures the levels of different types of cholesterol and triglycerides in your blood. High amounts of triglycerides, high LDL cholesterol, or low levels of HDL cholesterol are other components of metabolic syndrome.
Hemoglobin A1C
This blood test, also known as an A1C test, measures your glucose average over the past two to three months. The result is provided as an average of your glucose levels during that time. If your A1C level is higher than 5.7 percent, you are at risk for developing prediabetes or diabetes.
How Can You Lower Your Risk of Metabolic Syndrome?
If you’ve been given a diagnosis of metabolic syndrome, not to fear! By working with a healthcare professional and implementing healthy lifestyle habits, it may be possible to improve or reverse symptoms.
As Dr. Zachary shares, “lifestyle changes I would recommend to reduce one's risk of developing metabolic syndrome include:
- Improving diet quality
- Increasing physical activity and exercise
- Achieving or maintaining a healthy body weight
- Ensuring adequate sleep
Adopting these healthy lifestyle factors can help prevent or mitigate several components of metabolic syndrome, including excess abdominal obesity, high blood pressure, blood lipid abnormalities, and insulin resistance.”
Here are a few more tips to help you create healthier habits for metabolic health:

- Eat a healthy diet: Include plenty of fruits, vegetables, lean proteins, and healthy fats, and reduce things like ultra-processed foods, trans fats, added sugar, and alcohol. Working with a qualified nutritionist is a great way to make sure you’re following a balanced diet that’s suited to your nutritional needs.
- Exercise regularly: Being physically active can decrease your likelihood of being overweight and can help your body utilize insulin more efficiently.
- Get plenty of sleep: Sleep deprivation can lead to insulin resistance. Make sure to prioritize getting seven to nine hours of sleep per night.
- Reduce stress: Chronic stress is also a major contributor to impaired insulin sensitivity and can contribute to metabolic dysfunction. Taking steps to reduce stress can support better metabolic health.
Stop smoking: Smoking tobacco damages blood vessels and contributes to inflammation, which can increase your risk of heart disease.
Find the right Nutrisense programto turn insight into progress.
Metabolic Syndrome and Nutrisense FAQs
Q1. Can I use Nutrisense if I am concerned about metabolic syndrome risk but do not have diabetes?
A1. Yes. Nutrisense supports people without a diabetes diagnosis who want to understand how meals, activity, sleep, and stress relate to glucose patterns. Sensors measure glucose in interstitial fluid, and the app shows trends with 24/7 data, meal logging, and experiments. Dietitians can help interpret patterns and suggest habit changes that fit your life.
Source: CGM without diabetes
Q2. Do I need a prescription to start, and how quickly can I begin?
A3. No prescription is needed for the over-the-counter sensors used by Nutrisense. After signing up, approval typically takes 1 to 2 days. Orders processed in 1 to 2 days and shipped to U.S. addresses. Delivery usually takes 3 to 5 business days. You can schedule a nutritionist video call while you wait.
Source: How it works
Q3. Does Nutrisense diagnose or treat metabolic syndrome?
A5. No. Nutrisense provides wellness coaching and education to support healthy habits. It does not diagnose, cure, prevent, or treat any disease or medical condition. If you have symptoms or concerns about metabolic syndrome, consult your healthcare provider for evaluation and medical advice.
Source: Terms of Service
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. With Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
Build a Plan With Your Dietitian
Sign up to access insurance-covered video calls with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Data That Guides Your Choices
With the Nutrisense Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitors (CGMs), and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Start With Our Quiz
Ready to take the first step? Take our quiz to find the right Nutrisense program to help you take control.

Amanda is a Nutrition Manager and Registered Dietitian, with a Masters in Dietetics from Stephen F. Austin State University. Originally from south GA, she got her undergrad degree from Texas Tech University. She worked at a hospital in Fort Worth, TX, for 4 years as a dietitian, counseling those living with HIV.




