Glucose Monitoring: Understanding Time in Range (TIR)
Key Takeaways
Here at Nutrisense, we believe in glucose optimization and prioritizing a healthy metabolism. With our access to glucose biosensors and app that's compatible with many other continuous glucose monitors (CGMs), we help you track your glucose levels 24/7. You can then use this data to make healthy changes to your diet and lifestyle! However, before you can really start to make changes while wearing a CGM, you should first understand the metrics. If you’re new to the world of CGMs, here’s everything you need to know before you get yours.
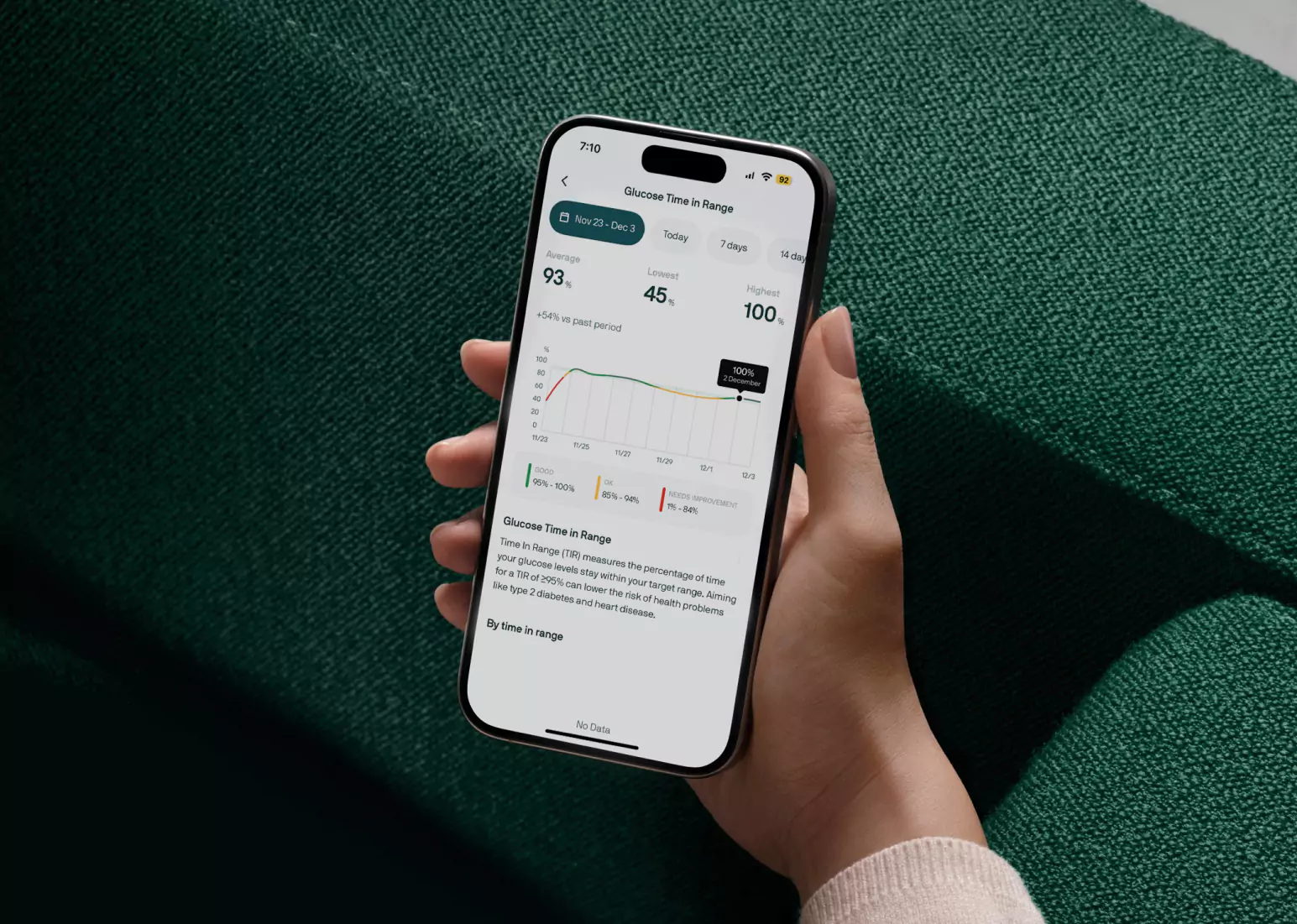
One thing you can measure with a CGM is something called time in range or TIR. In a nutshell: when you look at TIR, you’re measuring the percentage of time spent between a certain minimum and maximum threshold. This gives you a good idea of the total time your glucose is either above or below that set range, so you know exactly what you need to work on optimizing.
By now, you likely know we think wearing a CGM is not just for those with diabetes. In fact, even healthy people who check their glucose levels in a lab with tests like the A1C may not be getting the whole story. With non-diabetic glucose monitoring, you can get crucial information about what your glucose looks like in real-time versus at just one point in time.
This helps to keep glucose levels within normal limits. It’s like watching a movie versus looking at a photograph! In fact, if you’re looking at A1C alone, you may miss both hypoglycemic (time below range, or TBR) and hyperglycemic (time above range, or TAR) excursions that you can see through the time in range metric.
What is Time in Range?
Want to know a little more about the specifics of time in range? For starters, the common recommendation for TIR for those with type 2 diabetes is 70–180 mg/dL [3.9–10.0 mmol/L]. The goal is to limit both hypo and hyperglycemic excursions. Using your CGM may be an invaluable tool here! In fact, one recent study reported that those with type 2 diabetes could increase their TIR by 10 percent while wearing a CGM for 24 weeks.
A 10 percent increase in TIR also corresponded to a decrease in A1C of approximately 0.5 percentage points. Similar associations were seen in an analysis of 18 randomized controlled trials (RCTs). The American Diabetes Association (ADA) recommends those with type 2 diabetes stay in range for 70 percent of the day (or 17 out of 24 hours), either above or below the target range of 70-180.
For those without diabetes, few studies have looked at this directly. When studies are specific to those without diabetes (with average weight and health measures), they find that they remain below 140 mg/dL around 95-99 percent of the time. Those with diabetes tend to stay below 140 only 65 percent of the time. In a recent study, people without diabetes wore a CGM for 10 days.
The study found they spent about 96 percent of the TIR (set at 70-140 mg/dl), with glucose levels averaging between 98-99 mg/dl and showing little variation. Among participants who were over 60, the average glucose was 104 mg/dL. There also may be differences in how different genders process the same type of meals.
There’s an interesting study you can check out to find out more about this, which examined the differences in CGM values between men and women who ate the same meals for six days. It found that the percentage of values over the range of normal glycemia (> 140 mg/dL) in the postprandial period that they analyzed (six hours) was 9.7 percentage points in women and 7.1 percentage points in men. This suggests that different genders process the same meals differently, which could have interesting applications for assessing individual carbohydrate tolerance.
A1C vs. Time in Range

Remember that A1C measures average glucose levels over three months. It’s been seen as the gold standard when looking at glycemic control. However, because it is so dependent on the lifespan of the red blood cell (which is around 115 days but can vary), there can be some downsides. The lifespan of a red blood cell is affected by many things, including smoking, pregnancy, ethnicity, uremia, or anemia, all of which can skew the A1C value.
It also does not reflect any high or low blood sugar excursions or any variability in glucose levels throughout the day. This means that two people may have similar A1C values but different shifts or swings in their glucose levels throughout the day. It also does not identify how high your glucose is climbing after a meal. It’s crucial to have this information because, as some studies show, the risk for type 2 diabetes increases the more time non-diabetic people spend above a level of 140.
Interestingly, your A1C and TIR can inform each other. Looking through 18 studies, the authors of this study found a strong relationship between the two. For every 10 percent change in TIR, there was a correlating 0.8 percent change in the A1C value. Every hour above the range translates to an extra five percent shift in the TIR value, which is a significant change! This highlights the importance of looking at both an A1C and the data from the CGM.
Reasons Measuring Time in Range is Important For Monitoring Glucose

Can Be Measured At Home, Daily
An A1C value needs to be drawn by a medical professional at a lab or doctor’s office. The CGM, on the other hand, is a convenient (and painless) way to see what your glucose is doing in real-time. You can see your levels fluctuate during the day and in response to specific activities, meals, sleep, stress, and so on.
Allows You To See Direct Correlations Between Behaviors and Glucose Fluctuations
Glucose shifts through the day can impact everything from your mood to the amount of energy and cravings you have. Instead of looking at an A1C, which offers an average across a period, using the TIR metric with a CGM can give you information on-the-spot about how certain foods and behaviors impact glucose values.
For example, perhaps you ate an apple at 8 p.m. and saw a glucose spike above 160. This may also impact your A1C value, but with just an A1C test, you won’t know what you ate to cause this spike. However, you can see it reflected in the TIR value while wearing a CGM because that will reflect the actual number of hours you spent in and out of a set range during the day.
If you’re still not convinced, think of it this way: with a CGM, you can check an application on your phone to find out what your TIR is whenever you want. With an A1C test, you will have to wait for three months to pass to check it. Once you have this information, you can make specific tweaks to optimize any responses that cause glucose to spike above or below range.
More Time in Range Means Fewer Health Complications Related to Blood Sugar
Studies have shown that looking at TIR can help avoid complications in those with diabetes, especially microvascular complications like retinopathy or kidney disease. Those who spent less time in range and higher glycemic variability were more likely to have advanced diabetic retinopathy. In fact, TIR may be a better predictor of these complications than A1C. This is because it captures the direct impact of higher glucose values on the blood vessels and the swings in glucose. Recent evidence is also coming to light that glucose variability is directly tied to adverse health outcomes.
Different Time in Range Goals For Everyone

As we’ve gone over already, the TIR for glucose will look different based on various things. These include diverse populations, their health needs, medications, diets, lifestyles, and specific risk of hypoglycemia. It sounds confusing, but don’t worry, you don’t have to figure this out yourself. The ADA recently set some TIR goal recommendations for specific populations that you can refer to.
Time in Range For Healthy People Without Diabetes
Based on the current scientific evidence, we recommend trying to stay in range (between 70-140 mg/dL) at least 95 percent of the time when you’re using a CGM without diabetes to keep an eye on your levels. Remember that one percent of the time translates to <15 minutes, so we’re looking for less than 75 minutes a day spent out of range.
Time in Range During Pregnancy (With and Without Diabetes)
Current recommendations for pregnancy for those with type 1 diabetes are to stay between 63-140 mg/dL 70 percent of the time (more than 16 hours a day). Pregnant women with gestational or type 2 diabetes should aim to stay between 63-140 mg/dL for more than 90 percent of the time (or more than 21 hours).
Time in Range For People With Diabetes
For those with type 1 or type 2 diabetes, the goal is to stay between 70 180 mg/dL for more than 70 percent of the time (or more than 16 hours and 48 minutes) and more than 60 percent of the time for people less than 25 years old (or 14 hours, 24 minutes). For older populations or those with a high risk of developing diabetes, the recommendation is to stay in the range between 70-180 mg/dL more than 50 percent of the time (or more than 12 hours).
How Time in Range is Measured
To determine the TIR metric when wearing a CGM, you will want to go through at least 10-14 days of data. The CGM’ counts’ the time that your glucose was above, below, and in between a set range.
How to Improve Time in Range

While all this can sound like a bunch of confusing numbers and medical jargon, we’re here to help you make sense of your own TIR, so you can learn what changes you need to make to improve it. Start with a few of these easy tips to improve your TIR while wearing a CGM:
- Focus on your daily TIR rather than simply getting a good A1C value every couple of months. This will create a daily focus instead of an arbitrary goal to decrease your A1C value.
- Identify events that cause your glucose to shift out of range and then tweak them as necessary. For example, if a whole sweet potato made your glucose spike out of range, try a smaller portion, or try to time that type of carbohydrate around movement or exercise.
- Remember that every one percent out of range translates to 15 minutes. It can be helpful to set an attainable goal for yourself. Instead of simply saying, “I will improve my TIR,” you should know how that’s going to happen so you can make it happen! If you spend five percent of the time above range, focus on decreasing it to four percent by doing things like modifying your carbohydrate intake and pairing carbohydrates with fat/protein. You can also try getting more sleep, not eating too close to bedtime, and reducing stress levels.
- Check out this podcast that discusses helpful ways to biohack your glucose levels, which can ultimately help improve your TIR.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Amanda is a Nutrition Manager and Registered Dietitian, with a Masters in Dietetics from Stephen F. Austin State University. Originally from south GA, she got her undergrad degree from Texas Tech University. She worked at a hospital in Fort Worth, TX, for 4 years as a dietitian, counseling those living with HIV.




