What is Glucose Intolerance?

Key Takeaways
Monitor Patterns and Build Steady Habits
If you have glucose intolerance, you may be very aware of your glucose levels. Or, you may be concerned about your glucose levels and mindful of your symptoms, but unsure of how to monitor them.
Keeping track of your glucose values and ensuring you have normal glucose tolerance can be difficult, especially when glucose levels fluctuate throughout the day. Diet, exercise, hormones, sleep patterns, meal timing, medication, and stress all have an impact on your glucose levels.
If you are unsure of how these factors specifically affect you, it might be difficult to maintain balanced glucose levels throughout the day. A continuous glucose monitor (CGM) is a simple and effective way to monitor your glucose levels and understand the impact of various dietary and lifestyle factors on glucose levels.
Maintaining balanced glucose levels is key to lowering your risk for long-term health issues such as prediabetes or diabetes. Let's take a look at how you can determine if your glucose levels are out of balance.
What is Glucose Intolerance?
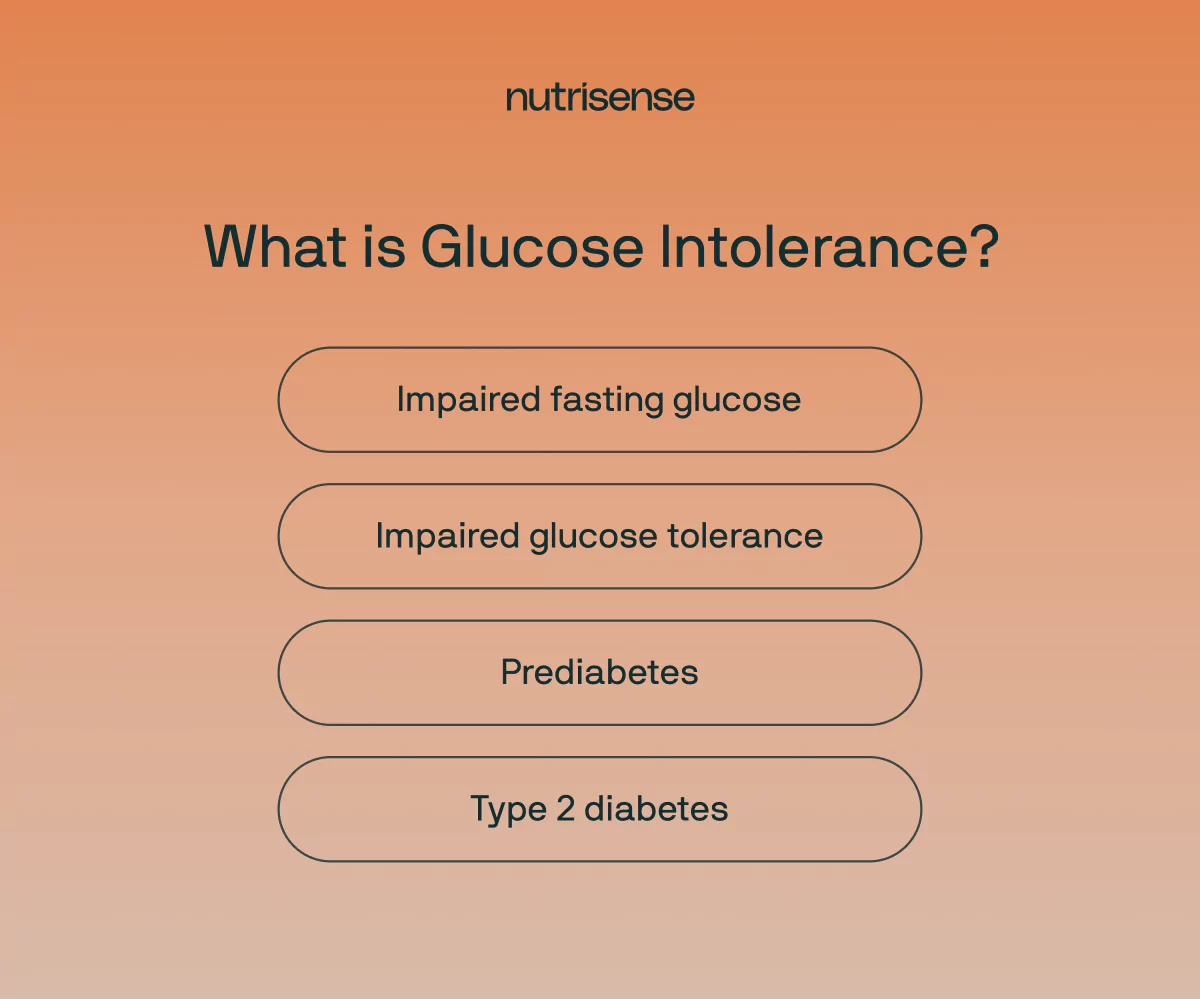
Glucose intolerance is a term that covers several metabolic conditions that cause abnormal glucose levels. These conditions include:
- Impaired fasting glucose (IFG): Also known as impaired fasting glycemia, metabolic syndrome, or prediabetes. This is when glucose levels are high during periods of fasting. However, glucose levels are not high enough to be considered diabetic.
- Impaired glucose tolerance (IGT): This is when your glucose levels are higher than normal but not high enough to be diagnosed as diabetic.
- Prediabetes: The term prediabetes is an umbrella term for both impaired fasting glucose and impaired glucose tolerance. Prediabetes will develop into type 2 diabetes in approximately 25 percent of people within three to five years. Up to 70 percent of people with prediabetes will become diabetic during their lifetime.
- Type 2 diabetes: This is the most common form of diabetes. It is a disease that occurs when your glucose is too high. Specific blood tests are carried out to diagnose type 2 diabetes.
What Causes Glucose Intolerance?
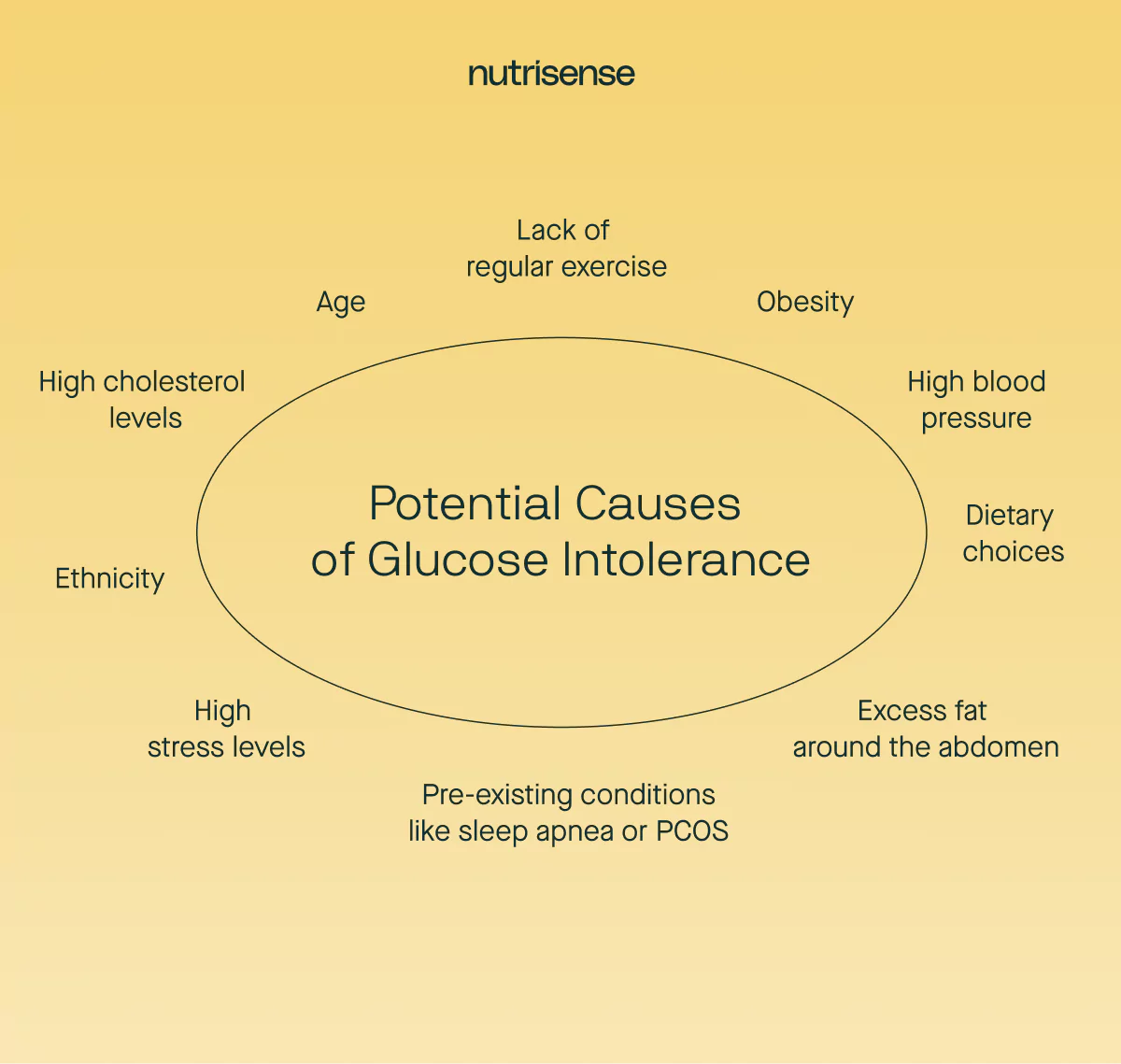
Glucose intolerance may have a number of contributing factors. Risk factors that increase the likelihood of becoming glucose intolerant include:
- Lack of regular exercise
- Obesity
- Excess fat around the abdomen
- High blood pressure
- High cholesterol levels
- Dietary choices
- Age (risk increases over the age of 45)
- Other pre-existing conditions, such as obstructive sleep apnea, gestational diabetes mellitus, and polycystic ovary syndrome
- Ethnicity (Black, Hispanic, American Indian, and Asian American people are at higher risk of developing prediabetes)
- High stress levels
What are the Symptoms of Glucose Intolerance?
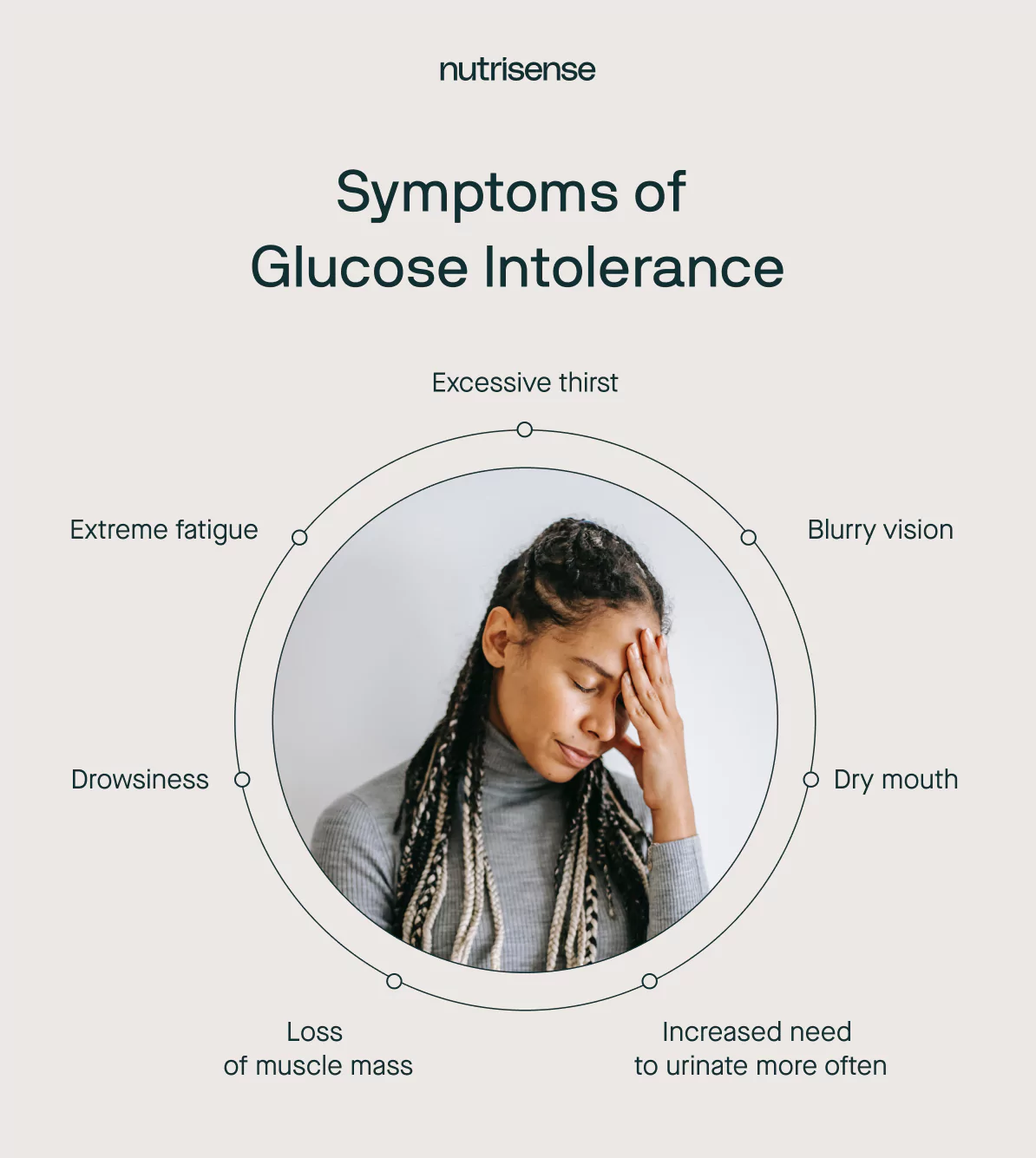
Many people with impaired glucose tolerance will not display any symptoms at all. However, if glucose intolerance is worsening or progressing toward diabetes, you may experience some symptoms.
That Mid-Morning Energy Slump
You start your day with a bowl of oatmeal and fruit, a choice that feels responsible. But an hour later, that familiar brain fog and drowsiness settle in, and you're fighting to focus through your morning meetings.
You’re left wondering why a seemingly healthy breakfast makes you feel like you need a nap before 10 AM. It’s this kind of confusion that makes understanding your body’s unique response so important, as one member shares: “I feel more confident and I think I'm healthier, and I understand how glucose works in my body.”
Here are some of the glucose intolerance symptoms to look out for that may indicate more concern for diabetes risk:
- Excessive thirst
- Blurry vision
- Dry mouth
- Extreme fatigue
- Increased need to urinate more often
- Drowsiness
- Loss of muscle mass
What's The Difference Between Glucose Intolerance and Diabetes?
You do not have to have a diagnosis of diabetes to be glucose intolerant. However, being glucose intolerant increases your risk of developing type 2 diabetes. Blood tests are used to distinguish between glucose intolerance and diabetes (see below).
What's The Difference Between Glucose Intolerance and Insulin Resistance?
Insulin resistance occurs when cells in your muscles, fat, and liver are less effective at responding to insulin. To compensate, the pancreas makes more insulin. This pancreatic response leads to high insulin levels in your blood.
If your pancreas produces enough insulin and your cells are able to respond to it, your body will be glucose-tolerant. However, if there is not enough insulin and/or your cells are unable to respond to it appropriately, the extra glucose stays in your bloodstream instead of entering your cells.
Over time, your cells may become more resistant to insulin. This can lead to a rise in both insulin and glucose levels. This is known as glucose intolerance.
{{rich-text-cta-cgm1="/style-guide"}}
What is a Glucose Intolerance Test?

There are three types of glucose intolerance tests. They are all blood tests.
- Fasting plasma glucose. This is a blood test taken after an eight-hour overnight fast to measure glucose levels.
- Oral glucose tolerance test (OGTT). This type of glucose test is done over several stages. First, a fasting blood sample is taken to get a fasting glucose reading. Secondly, you are given a syrupy pure glucose solution to drink. Finally, a healthcare practitioner will measure your glucose levels again two hours after drinking the solution. This tests your body’s ability to respond to elevations in glucose appropriately.
- Glycated hemoglobin. This blood test gives an average of your glucose levels over two to three months. The results from these blood tests are shown in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L).
What Test Results Indicate Glucose Intolerance?
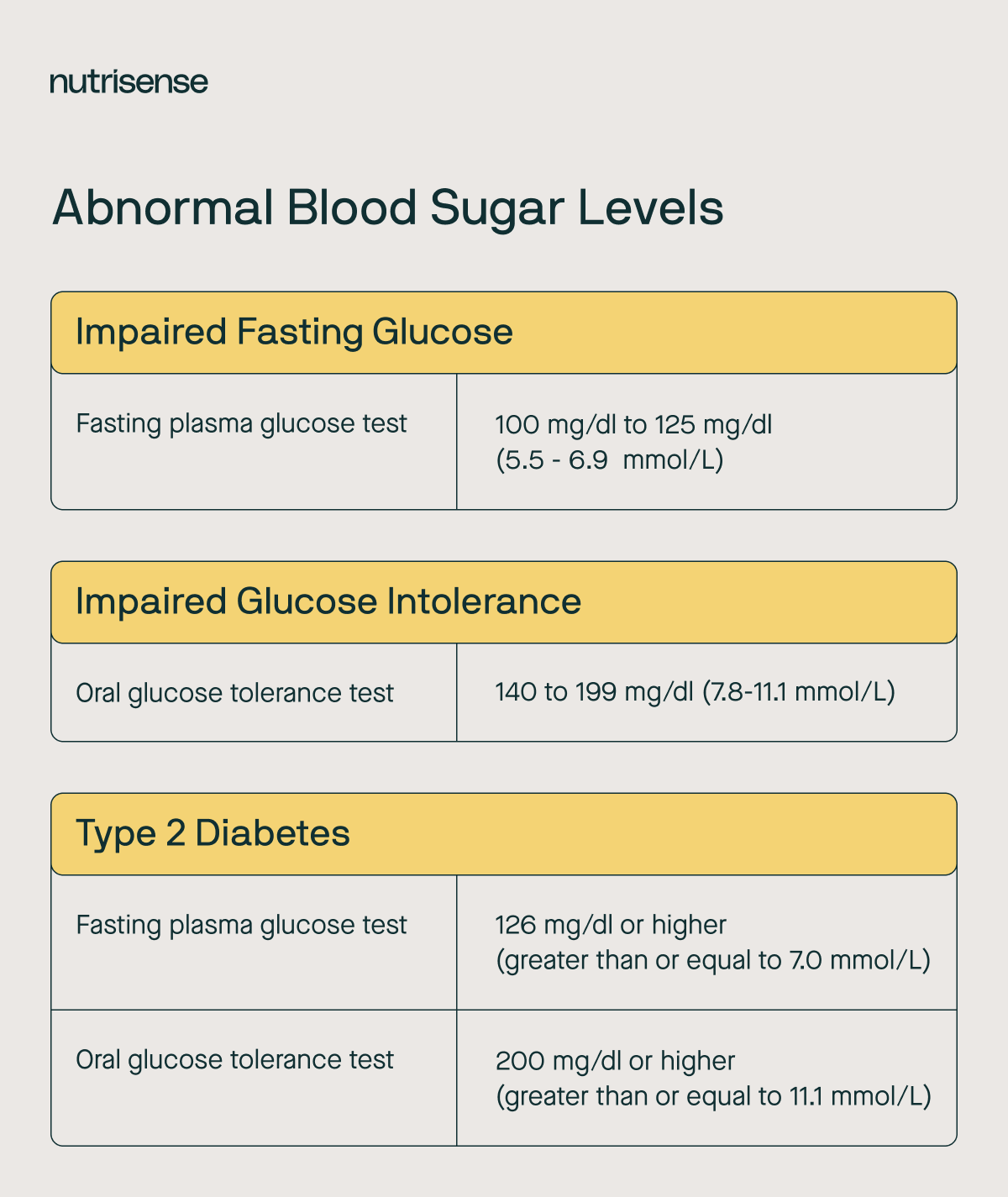
The recommended glucose levels for diagnosing diabetes and intermediate hyperglycemia (prediabetes) by the American Diabetes Association are as follows:
Impaired Fasting Glucose
- Fasting plasma glucose 100 mg/dL to 125 mg/dL (5.5 - 6.9 mmol/L)
Impaired Glucose Intolerance
- Oral glucose tolerance test 140 to 199 mg/dL (7.8-11.1 mmol/L)
Type 2 Diabetes
- Fasting plasma glucose 126 mg/dL or higher (greater than or equal to 7.0 mmol/L)
- Oral glucose tolerance test 200 mg/dL or higher (greater than or equal to 11.1 mmol/L)
Is There a Treatment For Glucose Intolerance?
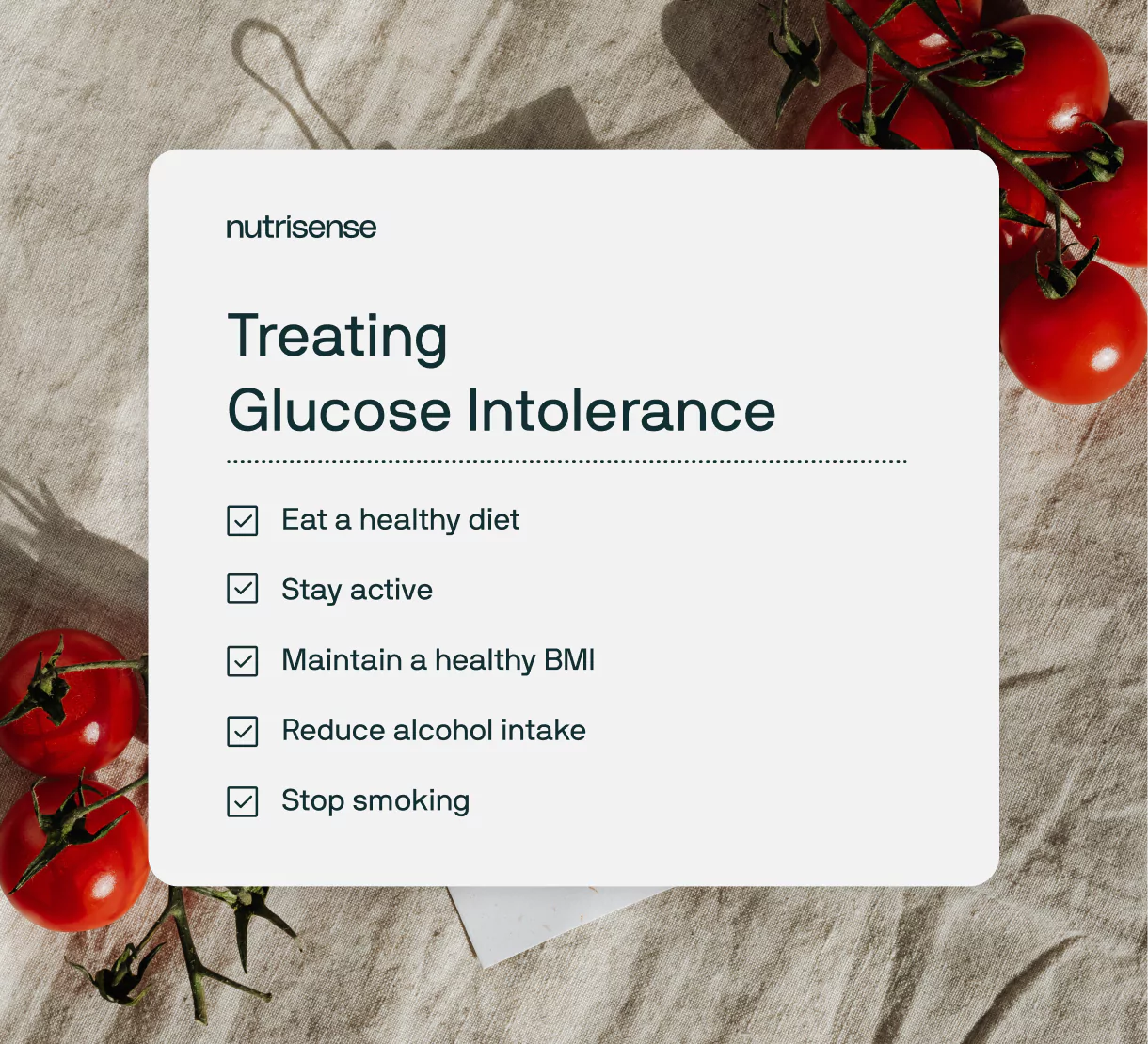
The treatment for glucose intolerance may differ depending on whether you have been diagnosed with IFG, IGT, or type 2 diabetes. Treatment includes lifestyle interventions, but in some cases, medication may be prescribed.
The following lifestyle modifications are recommended from the research:
1) Eat a Healthy Diet
Food such as ultra-processed foods and sugar-sweetened drinks is associated with an increased risk of type 2 diabetes. By comparison, consuming adequate protein from lean whole foods, non-starchy veggies, and high-fiber unrefined carbohydrates has been shown to reduce the risk of diabetes.
2) Increase Physical Activity
The CDC shows that exercise helps control your glucose levels. It also lowers your risk of heart disease and nerve damage.
3) Maintain a Healthy BMI
Body mass index is a measure of body fat based on height and weight that applies to adult men and women. According to the American Diabetes Association, being overweight not only raises your risk for type 2 diabetes but also for heart disease and stroke. Even a small amount of weight loss can make a big difference.
4) Reduce Alcohol Intake
Binge drinking and large quantities of alcohol can be harmful to many aspects of metabolic health. Too much alcohol may cause pancreatitis, which impairs the ability of the pancreas to secrete insulin. This, in turn, can potentially increase risk for diabetes.
5) Stop Smoking
The Food and Drug Administration (FDA) reports that smokers are 30 to 40 percent more likely to develop type 2 diabetes than nonsmokers.
Medication may be prescribed to help lower glucose levels. The most common medication prescribed is Metformin. Your doctor might also advise medication to control cholesterol or high blood pressure if these are additional problems that you have.
How Can I Reduce My Glucose Intolerance?

Using a CGM can help you monitor and understand your glucose levels throughout the day. This may allow you to gain insight into what diet and lifestyle factors impact your glucose levels.
Your body is unique and may respond differently to certain foods. Therefore, there is no way of knowing how each type of food impacts your glucose levels unless you are wearing a CGM and can observe what happens to your glucose levels 24/7.
Personalized Nutrition Plan
A CGM shows you how your glucose levels react to diet, exercise, medication, sleep, and stress. This allows you to develop a truly personalized nutrition plan and modify your lifestyle to reach optimal health.
Wearing a CGM will give you deeper insight into your overall metabolic health and help you better understand what factors impact your glucose levels. Once you develop an understanding of how your glucose levels react to your diet and lifestyle, you can alter your nutrition and daily habits accordingly.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. With Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
Talk to a Glucose Expert
Sign up to access insurance-covered video calls with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Track, Learn, Adjust
With the Nutrisense Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitors (CGMs), and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
See Which Plan Fits You
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Heather is a Registered and Licensed Dietitian Nutritionist (RDN, LDN), subject matter expert, and technical writer, with a master's degree in nutrition science from Bastyr University. She has a specialty in neuroendocrinology and has been working in the field of nutrition—including nutrition research, education, medical writing, and clinical integrative and functional nutrition—for over 15 years.




