Cold or Flu Impact on Blood Sugar: Unraveling the Connection

Key Takeaways
Most people are quite familiar with the typical symptoms of the common cold or the flu, but did you know that being sick can affect your blood sugar levels?
Most adults have an average of two to three colds per year, and roughly three to 11 percent of people get the flu every flu season. When you’re sick, your body releases stress hormones glucocorticoids, catecholamines, and pro-inflammatory cytokines to fight the infection. These hormones can raise your blood sugar, and your body may struggle to make enough insulin in response.
Whether or not you have diabetes, it’s important to be aware of how these common infections can affect your blood sugar as keeping your glucose levels stable can help you prevent potential complications and help your body to fight the illness more effectively..
Let’s take a deeper look at these common conditions and what they can do to your blood sugar levels.
What Causes the Common Cold?

The common cold is a contagious upper respiratory infection caused by a virus. Many types of virus can cause the common cold, but most are caused by rhinoviruses.
A cold virus gets into your body through your mouth, nose, or eyes, and is spread through droplets in the air when a sick person coughs, sneezes, or talks, and through hand-to-hand contact with contaminated objects or people who are sick.
Symptoms of the common cold include:
- Runny nose
- Congestion
- Sore throat
- Coughing or sneezing
- Mild body aches and/or headache
- Low-grade fever
While a cold tends to be mild, some more severe complications can arise. A cold can lead to other infections, such as ear or sinus infections, strep throat, or pneumonia.
Visit your doctor if your symptoms don’t improve or get worse, or you develop more serious symptoms like shortness of breath, wheezing, a fever higher than 103 fahrenheit, or severe headache or throat or sinus pain.
How is the Flu Different from the Common Cold?

The flu is also a contagious upper respiratory infection, and while its symptoms are similar to the cold, they are generally more severe and appear more abruptly.
The flu is caused by the influenza virus, and unlike the common cold, it can sometimes be prevented with a vaccine known as the flu shot.
Symptoms of the flu can include:
- Fever
- Chills
- Sore throat
- Coughing
- Runny nose
- Headache
- Fatigue
- Body aches
- Vomiting or diarrhea
More serious complications can occur, such as sinus or ear infections, pneumonia, and even inflammation of the heart, brain, or muscle tissue.
People who are aged 65 or older, children aged 5 or younger (but especially children aged 2 or younger), pregnant people, and people of any age with chronic medical conditions like diabetes, heart disease, or asthma, are all at higher risk of developing serious flu complications.
If your symptoms don’t improve or worsen, or if you are at higher risk of developing serious complications, visit your doctor. You may be treated with antivirals or other flu medications to help get symptoms under control.
How Does the Cold or Flu Affect Individuals With Diabetes?

In most cases, individuals with type 1 diabetes don’t make insulin, and people with type 2 diabetes aren’t able to properly use the insulin their body does make. Because insulin is required for the body to turn blood sugar into energy, it’s crucial for people with diabetes to monitor their blood sugar and take steps to keep it at their target levels.
Being sick with a cold or the flu can cause the body’s blood sugar levels to rise, so it’s important for people with diabetes to be extra mindful of their diabetes management during periods of illness.
Diabetic Ketoacidosis
Unchecked blood sugar levels can have severe effects when you have diabetes. When your blood sugar rises and your body doesn’t have enough insulin to process it, it starts to break down fat to use as energy, which produces ketones.
Too many ketones in your blood can cause diabetic ketoacidosis, or DKA, which can be life-threatening. In the early stages, DKA can make you thirstier than usual and urinate more than usual, but more severe symptoms can emerge if left untreated, such as:
- Dry mouth
- Fast, deep breathing
- Muscle stiffness or pain
- Fatigue
- Headache
- Fruity-smelling breath
- Nausea and vomiting
- Stomach pain.
When you have diabetes and are sick, or your blood sugar is 240 mg/dL or above, you can use an over-the-counter ketone test kit to check the ketone levels in your urine.
If your ketone levels are high, or you are experiencing any symptoms of DKA, call your doctor or go to the emergency room immediately as this condition needs to be treated right away.
Why Do Infections Increase Blood Glucose Levels?
During an immune response to illness or infection, extra glucose may be released into the bloodstream and serve as a defense mechanism for the body. Elevated blood glucose levels during infections are a natural reaction, supporting vital organs such as the brain, kidneys, and red blood cells that rely on glucose for energy. This process can thereby assisting the immune system in its response to combat the infection, and can be one reason why your glucose levels rise while you're sick.
How to Manage Your Blood Sugar When Sick
Anyone trying to optimize their health can benefit from monitoring glucose levels—you don’t have to have diabetes to learn about the benefits of optimizing your blood sugar response. Conditions like polycystic ovarian syndrome (PCOS), high blood pressure, Cushing’s syndrome, side effects of prescription medication, pancreatic diseases, and surgery or trauma can all lead to high blood sugar levels, also known as hyperglycemia.
Hyperglycemia can be unpleasant no matter why you are experiencing it, but there are a few things you can do to manage it during periods of illness.
Check Your Blood Sugar Often
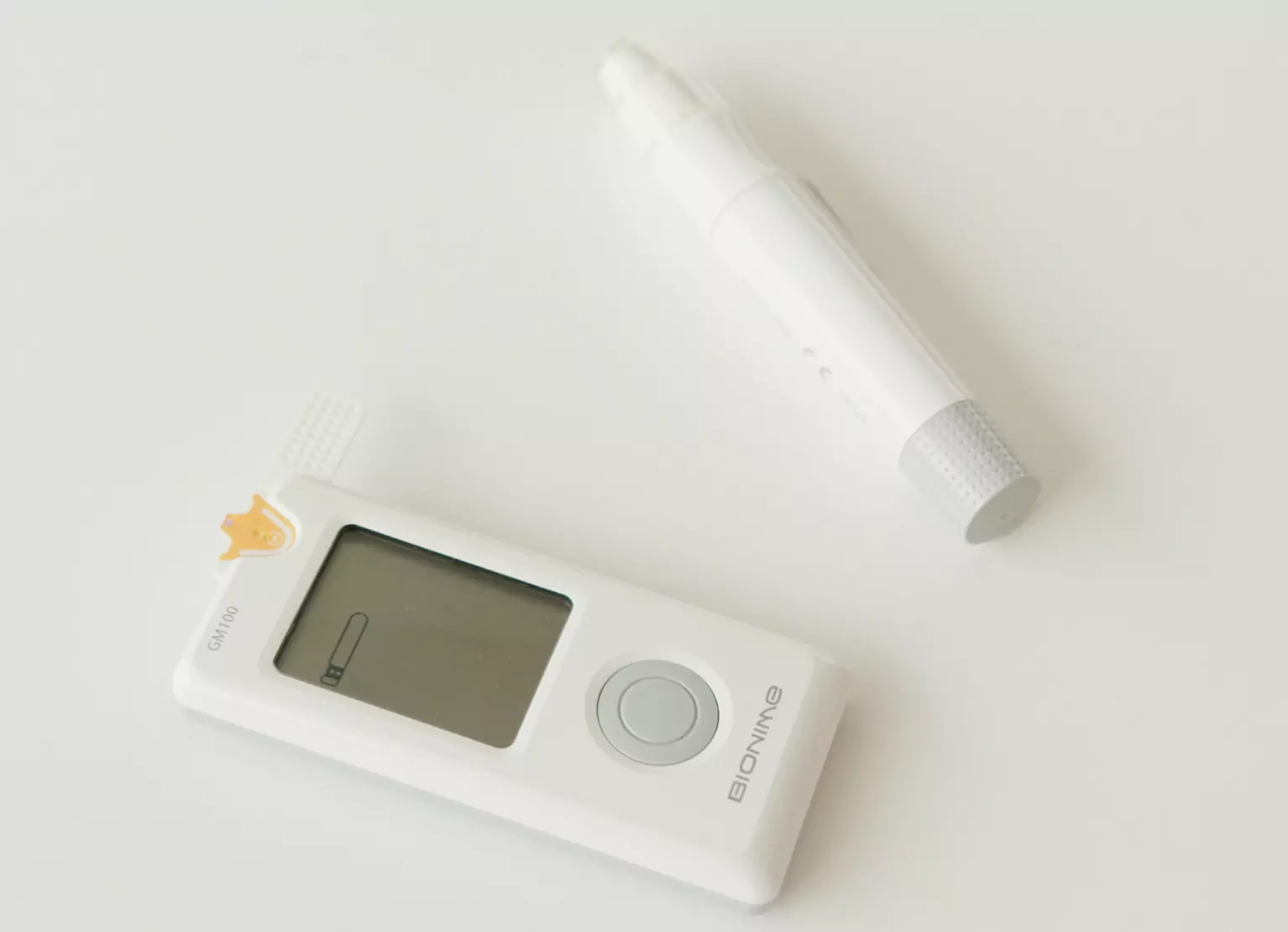
If you’re someone with diabetes, you may choose to check your blood sugar regularly to see how your body is responding to your illness. One way to track your blood sugar is to use a continuous glucose monitor, or CGM, which is a small, painless device that attaches to your arm.
If you have diabetes and are worried about DKA, it is recommended that you check your blood sugar every two hours.
Be Aware Of Ingredients In Your Cold Medicine
Some over-the-counter medications contain elements that can raise your blood sugar, such as decongestants, while other medicines such as aspirin and Tylenol contain inactive ingredients that can lower your blood sugar.
Talk to your doctor or a pharmacist to determine which medicines are safe for you to take.
Keep Taking Your Usual Medications
When you’re sick, it’s important to keep taking your usually prescribed medication, even if you can’t eat. If you feel like you may need to adjust any diabetes medication while you’re sick, contact your healthcare provider.
Do not adjust your medication or insulin without instruction from your doctor or healthcare professional.
Drink Plenty Of Fluids
It’s important to drink a lot of fluids to replace any water you’ve lost because of your illness. Being sick can cause dehydration, especially if you’ve experienced diarrhea or vomiting. High blood sugar can also cause more frequent urination, which can lead to further dehydration.
Stick to water and low-sugar drinks, such as unsweetened herbal tea. The CDC recommend drinking four to eight ounces of fluids every half-hour.
Eat Regular Meals
It’s also important to try to eat regular meals, even when you are sick. Try to eat as often as you normally would, especially if you’re following a diabetes diet or a meal plan that is meant to manage your blood sugar.
Reaching your regular daily calorie intake while continuing to consume adequate protein while sick can help make sure your body has enough energy to fight the infection. If you find it hard to keep up with your normal diet, try eating whole foods such as plain Greek yogurt, bone broth, soups or stews regularly.
If you are unsure about what to eat to manage your blood sugar while you’re sick, or if you’re having trouble eating, contact your healthcare provider for specific advice and recommendations.
Create A Sick Day Plan

If you’re someone with diabetes, it may be a good idea to have a plan in mind before you get sick so that you are well prepared to manage your blood sugar during times of illness. Talk to your healthcare team to figure out a strategy that includes:
- How often you should check your blood sugar
- What foods to eat while you’re sick
- What fluids you should be drinking, and how often
- When you should call your doctor
- When you should check for ketones
- Which over-the-counter medications are safe for you to take
Having this information on hand when you get sick can make your life a lot easier, and take a few hard decisions off your plate.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Carlee's training at Western Illinois University and an internship at the Memphis VA Hospital lead her to a career in outpatient counseling and bariatric nutrition therapy. In these positions, Carlee realized many of the disease states (upwards of 80%!) her patients experienced were actually preventable. She knew she had to dig deeper into preventative health and has since been passionate about helping people translate this complex glucose data into actionable changes anyone can implement into their everyday lives.




